Africa, The "Forgotten" Monkeypox Outbreak
Unlike In The Global Outbreak, People Are Actually Dying There
Virtue signaling is one of the more nauseating features of the “woke”—especially when it is infected (as it usually is) by a toxic mixture of ignorance and hypocrisy.
The monkeypox “emergency” is a narrative that seems built entirely on such virtue signaling. How else can one comprehend the bizarre dismissal of literally thousands of monkeypox cases and well over 100 deaths, while all the while pontificating and posturing over the “failure” of healthcare systems to provide sufficient quantities of smallpox monkeypox vaccines to LGBTQ+ communities even as stern lectures are given not to “stigmatize” monkeypox as a “gay” disease (which, by the way, it isn’t—what it is outside of Africa is an STD analogous to herpes, and like all STDs is spread through promiscuous and unsafe sex, period)?
Monkeypox By The Numbers
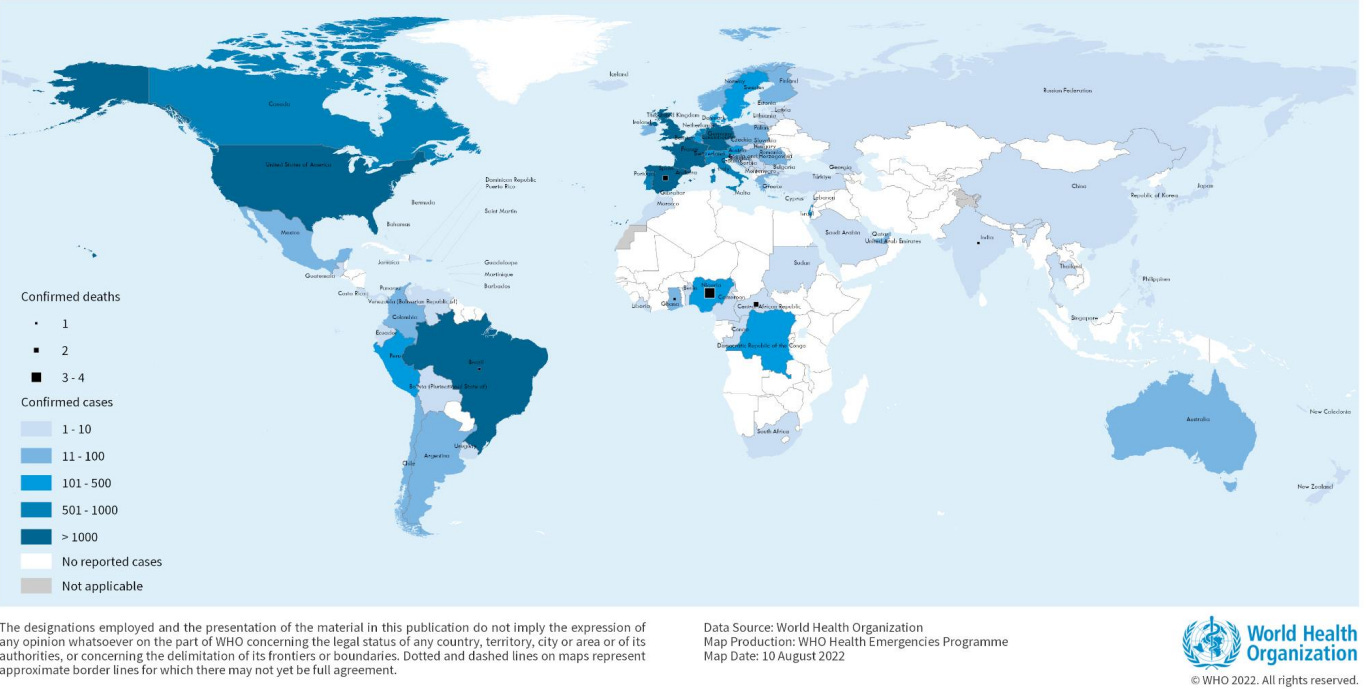
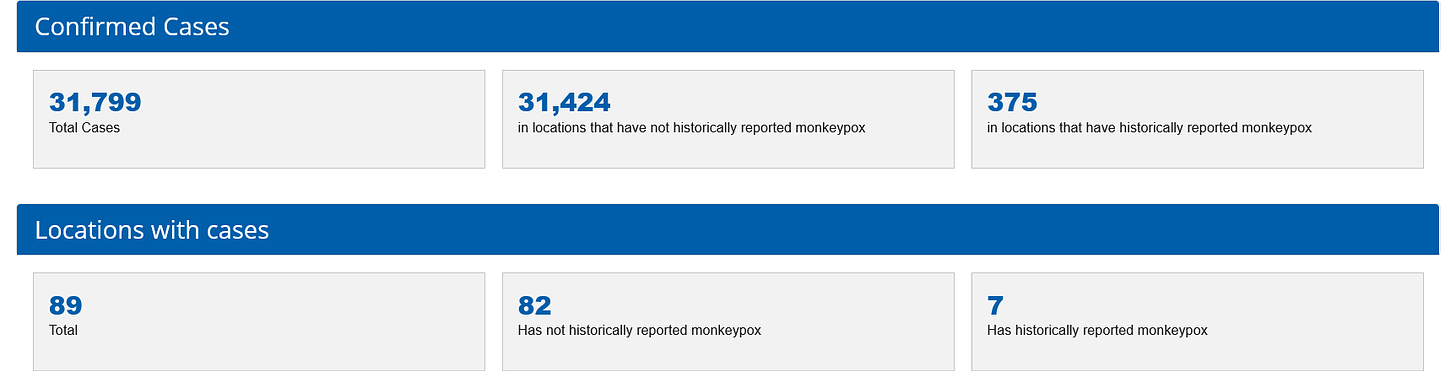
According to the CDC, as of August 12, 2022, there are 31,799 confirmed cases of monkeypox worldwide. 31,424 of those cases are in countries where monkeypox has historically not been reported, leaving only 375 of those cases within monkeypox’ historic endemic region.
11,177 cases of monkeypox are here in the United States.
The CDC reports a total of 12 deaths attributed to monkeypox—5 outside of monkeypox’ historic endemic region and 7 within it.
Within the United States, the disease is heavily concentrated among gay and bisexual men with close (i.e., sexual) contact between infected and non-infected men being the likely mode of transmission1.
Among the male patients with information on sexual activity, 99% (n=624) reported male to male sexual contact. Approximately 38% (n=524) of patients with known race/ethnicity are white/non-Hispanic, 26% (n=358) are Black, and 32% (n=445) are Hispanic (of any race). Data are missing for a large number of cases.
Note that the virus does not appear to be discriminating against any one minority or demographic.
Africa’s “Forgotten” Cases
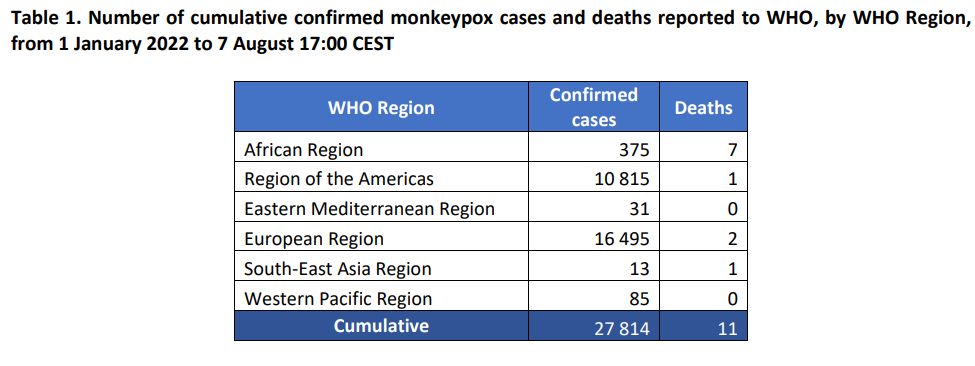
The WHO’s most recent Situation Report on the global monkeypox outbreak shows similar data. The differences in case counts are attributable to having different cutoff dates for inclusion in the count.
Note that even by both the WHO and CDC data, the majority of deaths from monkeypox are occurring in Africa.
However, look at the actual case counts that are reported to the WHO’s regional office in Africa:
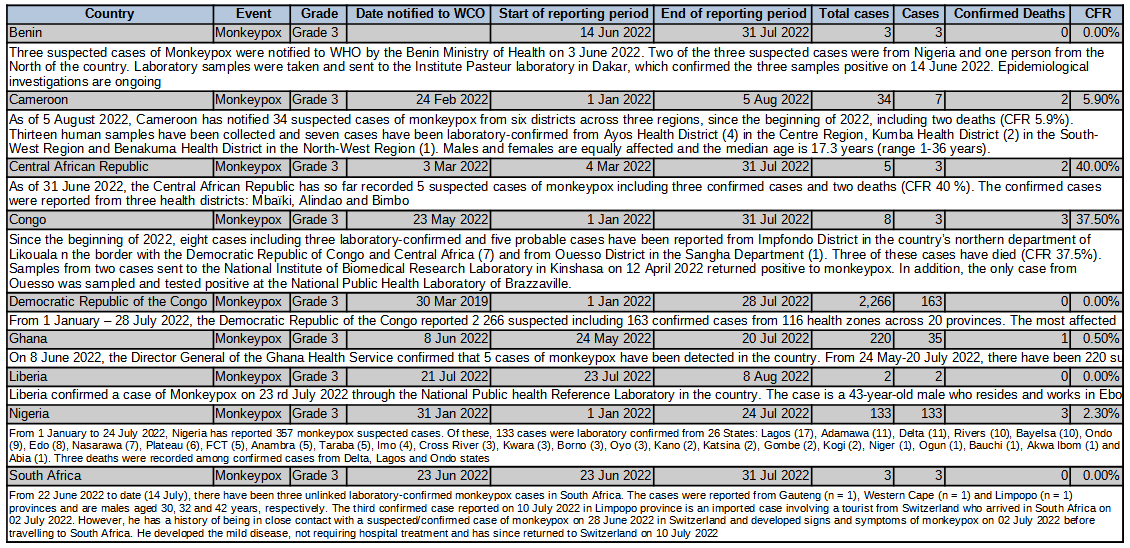
Including suspected cases, there are 2,674 monkeypox cases within Africa and 11 “confirmed” deaths as of the most recent weekly bulletin (Bulletin 32, 1-7 August 2022). The confirmed attribute is relevant because up through WHO-Africa’s Weekly Bulletin on Outbreaks and Other Emergencies Number 30 (18-24 July 2022), suspected deaths were being reported as well, and the Democratic Republic of the Congo had 65 suspected deaths as of that report period. Reporting after that only counted confirmed deaths.
Intriguingly, Weekly Bulletin 31, the first bulletin focusing on confirmed deaths (and thus dropping the DRC deaths to 0), came right after the WHO declared monkeypox a Public Health Emergnency of International Concern on July 23.
Including all suspected cases there are reports of nearly 3,000 cases of monkeypox in Africa, and over 100 deaths just in 2022.
At least 2,947 monkeypox cases have been reported in 11 African countries this year, including 104 deaths, but most of the cases reported are suspect ones because the African continent also lacks enough diagnostic resources for thorough testing, the Africa CDC director said.
It is worth noting that at least 81 people died from suspected monkeypox in the Democratic Republic of the Congo during 2021, another 229 died in 2020, and 107 more died in 2019.
Since epidemiological week 1 up to week 49 in 2021, 2 898 cases have been reported with 81 deaths (CFR 2.8%). Between epidemiological week 1 and week 53 of 2020, a total of 6 257 suspected cases including 229 deaths (CFR 3.7%) were reported in 133 health zones from 17 out of 26 provinces in the country. During the same period in 2019, 5 288 suspected cases and 107 deaths (CFR 2.0%) were reported in 132 health zones from 18 provinces. Overall, there was a regressive trend from epidemiological week 33 to 53 of 2020 (276 cases vs 76 cases)
However, despite having the most confirmed deaths from monkeypox in 2022, as well as hundreds of suspected deaths just in the DRC since 2019, Africa has at this time zero doses of the Jynneos smallpox vaccine2, which is currently the only FDA-approved vaccine for monkeypox3.
Africa’s Centers for Disease Control has been trying to obtain doses of Jynneos, but thus far without much success. The Africa CDC is in direct talks with at least two agencies outside of Africa and outside of government, but talks are not the same as vaccine doses.
This even as a clinical trial for Jynneos within the Congo is underway.
But a clinical trial is underway in Congo for a vaccine, Jynneos, that's under emergency use authorization, Ogwell said. The two-dose vaccine is considered the main medical weapon against the disease, but its availability is limited. The Africa CDC did not immediately respond to a question about details of the trial.
With some African countries reporting a case fatality rate of 37.5% just among confirmed deaths4, if any place can make a credible claim for increased need for the Jynneos vaccine, it is Africa. While the disease is not spreading as fast within its historic endemic region as it is elsewhere, it has been considerably more lethal, as the mere 5 deaths thus far among the 31,000+ cases of monkeypox recorded outside of Africa--as opposed to 100+ deaths among ~3,000 cases just this year alone within Africa--illustrates.
Yet while the African outbreak is demonstrably more lethal than the overall global outbreak, the WHO has been careful to minimize and even conceal the severity of the disease in Africa. Subsequent to the June 10 Disease Outbreak News bulletin on monkeypox, the WHO simply discontinued reporting suspected cases and suspected deaths within Africa, while the WHO’s regional office for Africa did the same for suspected deaths starting with Weekly Bulletin on Outbreaks and Other Emergencies Number 31. With just a few keystrokes, the WHO literally made hundreds of suspected monkeypox deaths in Africa just disappear.
For its part, the corporate media in the US has regarded the African outbreak largely as a footnote to the global outbreak, with the admittedly unusually rapid spread of the virus among gay and bisexual men capturing by far the majority of the media’s attention.
Not One Outbreak, But Two
A point I have made before, and which subsequent data only serves to emphasize even more, is that the African outbreak is substantially different from the global outbreak outside of Africa—so much so that it is inappropriate to consider the African cases as part of the same outbreak as the global cases.
Consider just a few of the important distinctions:
As I have discussed previously, there is data indicating the monkeypox strain involved in the global outbreak has 47 single nucleotide substitutions (mutations, in other words) differentiating it from its closest identified ancestral strain from Nigeria’s outbreak in 2017.
That data also suggests the global outbreak may have emerged in 2017, and has merely been ignored until this year.
Another point that I have touched on previously, the lesions appearing in cases within the global outbreak have a different appearance from the lesions associated with the pre-existing outbreak in West Africa.
Sexual contact does not appear to be a factor in the African cases, yet it is a defining characteristic among the European and North American cases, where more than 98% of the reported cases are among gay and bisexual men (“men who have sex with men”, in the current PC argot).
Much of this has already been acknowledged by the medical research community, which has managed to overlook the medical and scientific relevance of these and other differences while using them to make a case for adding new clades to the existing monkeypox taxonomy and renaming monkypox so that the name will not “stigmatize” infected individuals.
Even the corporate media touches on the divergent natures of the African and global outbreaks even as it glosses over the differences, leading to such mis-aligned statements by the media as this:
More monkeypox deaths have been reported on the African continent this year than anywhere in the world. Since May, nearly 90 countries have reported more than 31,000 cases.
Note the subtle shift from “deaths” to “cases”? Lost is this sublime conflation is the reality that, when one includes suspected cases and deaths, more than 90% of monkeypox deaths this year are in Africa.
For its part, the WHO has been subtly but persistently working to “memory hole” the unconfirmed “suspected” monkeypox cases in Africa, thereby downplaying the extent of the outbreak in West and Central Africa. The most notable example of this is the decision by the WHO to discard the suspected African cases previously reported from the Disease Outbreak News Bulletin of June 17.
At every turn, a deliberate and demonstrable effort has been made to obscure the distinct African outbreak by subsuming it into the global outbreak, ignoring the multiple differences between the outbreaks to present them as one outbreak rather than two.
Losing Important Context
By incorporating the African outbreak into the global outbreak of monkeypox, the corporate media and public health “experts” pushing the narrative on monkeypox have successfully guided the public’s attention on the disease away from the far greater mortality in Africa and towards the far greater pathegenicity outside of Africa.
What I have stated before I shall repeat here: The African monkeypox outbreak lends important context to understanding the nature of the global monkeypox outbreak. The spread of monkeypox within Africa is happening by different transmission vectors, is impacting a different patient demographic, and involves a distinctly different strain of the monkeypox than what is spreading globally. The monkeypox strain within Africa, based on what has been reported, presents noticeably different lesions than the strain spreading globally.
Just as there are already West African and Congo Basin clades of the virus, it is hardly a leap of logic to infer there is at least one other clade which encompasses the global outbreak. How and when those clades came to be greatly impact the question of where those clades came to be—did they arise in or out of Africa?
The prevailing presumption is that smallpox vaccination—which Jynneos is—provides protection against monkeypox. However, the research establishing 85% efficacy for smallpox vaccines against monkeypox is limited to observational studies from the 80s charting the course of monkepox outbreaks after smallpox vaccinations were discontinued in Africa5.
As Igor Chudov examines in his Substack, even that 85% assessment may not be all that accurate. That figure is only going to be further challenged by the degree of mutation/evolution of the monkeypox virus going from the West African clade to the clade(s) involved in the global outbreak.
Studying and understanding the differences between the two outbreaks of monkeypox are the essential foundation for effectively mitigating, treating, and ultimately stopping both. That’s what good science would do and should be doing.
That good science requires one to begin by acknowledging and focusing on the reality that there are two monkeypox outbreaks, not one, a context that is lost when one attempts to shoehorn the African outbreak into being simply a part of the global outbreak.
Monkeypox Is Not HIV
One truth about monkeypox should be intuitively obvious: monkeypox is not HIV. Within the globally spreading clades, the case fatility rate is infinitesimal, with 5 recorded deaths thus far against 31,000+ cases. Even for the clades behind the African outbreak the case fatality rate is only ~3-6% when all cases, suspected and confirmed, are included. While even a 3% case fatality rate is extremely high compared to the vast array of other diseases to which humans are susceptible, at the same time it is far from the eventual certainty of death from HIV once it develops into AIDS6.
The mortality risk to the LGBTQ+ community from monkeypox is still extremely low, based on the data. The mortality risk within Africa from monkeypox is higher by several orders of magnitude. People are dying and continuing to die from monkeypox in Africa. As of this writing that same statement cannot be said about the spread of monkeypox beyond Africa.
If the concern is truly for the health and welfare of human beings, without discrmination or prejudice or “stigma”, should not the activism about monkeypox be directed towards assisting the populations most at risk from the disease—the denizens of western Africa?
While the level of obligation of assistance from the US to countries in Africa regarding monkeypox or any other infectious disease is always a matter of much debate—as it should properly be—the demonstrated lethal potential for monkeypox in Africa means there should at least be that debate. That debate does not include the gratuitous use of monkeypox to rehash HIV and AIDS treatment policies from decades ago.
Sadly, such gratuitous virtue signalling is all we seem to get about the disease.
Technical Report: Multi-National Monkeypox Outbreak, United States, 2022 . 28 July 2022, https://www.cdc.gov/poxvirus/monkeypox/clinicians/technical-report.html.
Jynneos has never been rigorously tested in the field against either smallpox or monkeypox, and its efficacy against monkeypox is largely educated guesswork based on immunogenicity tests and animal trials.
The FDA approved Jynneos for monkeypox at that same time it approved the vaccine for smallpox. The efficacy data supporting both approvals was the immunogenicity results from clinical trials.
Because the number of confirmed cases are low, the case fatality rates are most probably overstated. Historically, the fatality rate for the West African clade of monkeypox is 0-6%, and the the fatality rate for the Central African clade is 10-11%
Fine, P E et al. “The transmission potential of monkeypox virus in human populations.” International journal of epidemiology vol. 17,3 (1988): 643-50. doi:10.1093/ije/17.3.643
Zwahlen M, Egger M: Progression and mortality of untreated HIV-positive individuals living in resource-limited settings: update of literature review and evidence synthesis. 2006, UNAIDS Obligation HQ/05/422204.



The removal of the suspected cases in Africa is interesting. My interpretation of this change is that it provides cover for certain demographic groups to keep all of the vaccine doses in Western countries. If the risk profiles look the same everywhere then there is no longer the pressure to send limited vaccine supplies there. Stability of reporting practices is so important when assessing time series. It becomes very difficult to properly assess risk in the absence of it. National and world agencies have done their best job during the past couple years to obscure data.
"Note that the virus does not appear to be discriminating against any one minority or demographic."
Well thank heavens for that!
I still would feel better if we had at least some clue about what modifications were done to the smallpox virus to "weaponize" it by not just former Soviet scientists but western ones as well.
Literally any of the classified research, development, testing would/could be invaluable to researchers today, and although it should be more than clear enough we as a species need to get beyond this biowarfare fascination, it looks less likely now than at any other time.
Fantastically well done article, PNK!