The BA.2 "Surge": A Case For Passive Surveillance
BA.2 Is Already Endemic. Alarmist Approaches Are Inappropriate
Pandemic Panic would be lost without a daily dose of fear in the propaganda, and today’s dose comes courtesy of the Los Angeles Times’ scarifying headline about how “Omicron subvariant BA.2 spreading rapidly in L.A. and across the nation“
The percentage of Omicron subvariant BA.2 cases is rising in Los Angeles County, a trend seen elsewhere nationwide as officials sound the alarm about Congress’ failure to provide critical funding for vaccinations, tests and anti-COVID drugs.
As readers of this Substack may recall, this “outbreak” is the second time in the spotlight for BA.2. Last month we discussed how the “study” purporting to show the dangers of Omicron BA.2 was all theory and no reality.
The rise of BA.2 has also occasioned the return of Anthony “The Science™” Fauci to the airwaves to predict that BA.2 will soon impact the whole of the United States.
Fauci said the variant, which is already dominant in some European countries, is 50% to 60% more transmissible than Omicron. Currently BA.2 makes up roughly one third of COVID-19 cases in the United States but will likely overtake Omicron this spring.
However, as has been true repeatedly throughout the two-years-and-running of the Pandemic Panic Narrative, the data tells a rather different story.
The PERCENTAGE Of BA.2 Is Rising. Total Cases Are Not.
The first problem we encounter with the LA Times article is one of straight up credibility. The first several paragraphs make repeated reference to “rising percentages”:
According to data released Thursday, 14.7% of coronavirus samples analyzed for L.A. County between Feb. 27 to March 5 were the highly contagious BA.2 subvariant. That’s more than double the previous week’s figure of 6.4%.
However, Los Angeles County’s own dashboard does not show cases to be rising at all, but falling.
As a matter of basic math, a “rising percentage” of case totals which are declining merely means that BA.2 is diminishing more slowly than other variants—BA.2 will be the last variant out the door in Los Angeles, and hopefully it remembers to turn out the lights!
The LA Times goes on to imply that BA.2 cases are rising across the country:
More recent national estimates have suggested BA.2 will quickly become dominant soon. BA.2 comprised an estimated 35% of analyzed samples between March 13 and March 19; the previous week, it made up 22%, according to the U.S. Centers for Disease Control and Prevention.
In the Southwestern U.S. — which includes California, Arizona, Nevada and Hawaii — BA.2 made up an estimated 41% of coronavirus samples. The previous week, it was 28%. And for the first time, BA.2 is the now estimated to be the dominant subvariant in the Northeast, making up more than half the analyzed coronavirus cases in New York, New Jersey and New England.
However, this implied rise in cases also does not conform to the data. In New York City, for example, which recently reported a slight increase in cases, not only are the case numbers a mere fraction of what they were for the Omicron BA.1 variant, the hospitalization numbers continue to drop.
An incremental uptick in case counts with a declining number of hospitalizations is hardly a public health crisis, regardless of what the LA Times opines.
Moreover, as has already been discussed, Omicron BA.2 has been present in the United States for at least three months without a major rise in cases. If BA.2 is more transmissible than BA.1, why hasn't the US seen more BA.2 cases than it has?
If cases are broadly declining—and the data indicates this is so—how can there be a “surge” of BA.2 cases, or indeed of any COVID-19 cases?
“Experts” Are Having Withdrawal Symptoms Now That Endemicity Is Undeniable
What the media is actually showing is how the nation’s public health “experts” are experiencing withdrawal symptoms now that Pandemic Panic has receded with the Omicron wave, and are attempting to cope by drumming up phantom fear over “the next” surge. Indeed, what is being reported in the LA Times echoes a theme picked up by the Associated Press:
Despite disease monitoring improvements over the last two years, they say, some recent developments don’t bode well:
—As more people take rapid COVID-19 tests at home, fewer people are getting the gold-standard tests that the government relies on for case counts.
—The Centers for Disease Control and Prevention will soon use fewer labs to look for new variants.
—Health officials are increasingly focusing on hospital admissions, which rise only after a surge has arrived.
—A wastewater surveillance program remains a patchwork that cannot yet be counted on for the data needed to understand coming surges.
—White House officials say the government is running out of funds for vaccines, treatments and testing.
In order to have a fuller understanding of what is being reported, it is important to understand how the CDC uses (and, apparently, has used) the term “endemic”.
The amount of a particular disease that is usually present in a community is referred to as the baseline or endemic level of the disease. This level is not necessarily the desired level, which may in fact be zero, but rather is the observed level. In the absence of intervention and assuming that the level is not high enough to deplete the pool of susceptible persons, the disease may continue to occur at this level indefinitely. Thus, the baseline level is often regarded as the expected level of the disease.
This definition is reflective of the dictionary definition of the term: “belonging or native to a particular people or country”.
By the dictionary definition, a pathogen (or any organism) is “endemic” when it becomes native to a region, and exists there more or less indefinitely without additional importations of individual members of the species (in this case, virion particles). The CDC nuances this to indicate that a pathogen is “endemic” when it exists at a base level that is not extraordinarily disruptive to human lives; as Stuart Ray, professor of medicine at Johns Hopkins stated in a January article in the Washington Post:
In simpler terms, it means “a point at which the infection is no longer unpredictably disruptive,” said Stuart Ray, a professor of medicine in the division of infectious diseases at Johns Hopkins.
The lifting of COVID-19 restrictions and mandates, the calls for ending mask mandates for air travel, and the ending of “Zero Covid” protocols even in such infamously restrictive places as New Zealand, indicates the world is accepting the endemicity of the SARS-CoV-2 virus and the associated disease COVID-19. The “experts” and their acolytes in the corporate media are not happy with this, and would like to change people’s minds.
But despite the collective desire to move on, the pandemic is not over. Roughly one thousand people are still dying of the virus per day, and Covid-19 is the third-leading cause of death in the United States. Only 65 percent of the population is fully vaccinated, and 44 percent have received booster shots. Children under the age of 5 are still ineligible to receive vaccines. Millions of immunocompromised Americans must now navigate a reopened society, and the full effects of so-called “long Covid” are still unknown. The coronavirus is not yet endemic, the stage that would mean the virus is constantly present but manageable, like the seasonal flu. Far from receding, in fact, cases are once again on the rise in Europe because of the BA.2, or “stealth” omicron variant, which the White House on Monday acknowledged has begun to circulate in the U.S.; Europe has long foreshadowed our own pandemic trends.
However, the media, as is their habit, keeps tripping over inconvenient facts. The same AP article that bemoaned the lack of funding for Pandemic Panic without end also noted that BA.2 has been in the US since at least mid-December 2021.
For example, scientists this week touted a 6-month-old program that tests international travelers flying into four U.S. airports. Genetic testing of a sample on Dec. 14 turned up a coronavirus variant — the descendant of omicron known as BA.2 — seven days earlier than any other reported detection in the U.S.
BA.2 has been in the US since before Christmas and there has yet to be signs of a major uptick in cases. Perhaps this is a hint that this variant will not be “Omicron 2.0”, at least not yet?
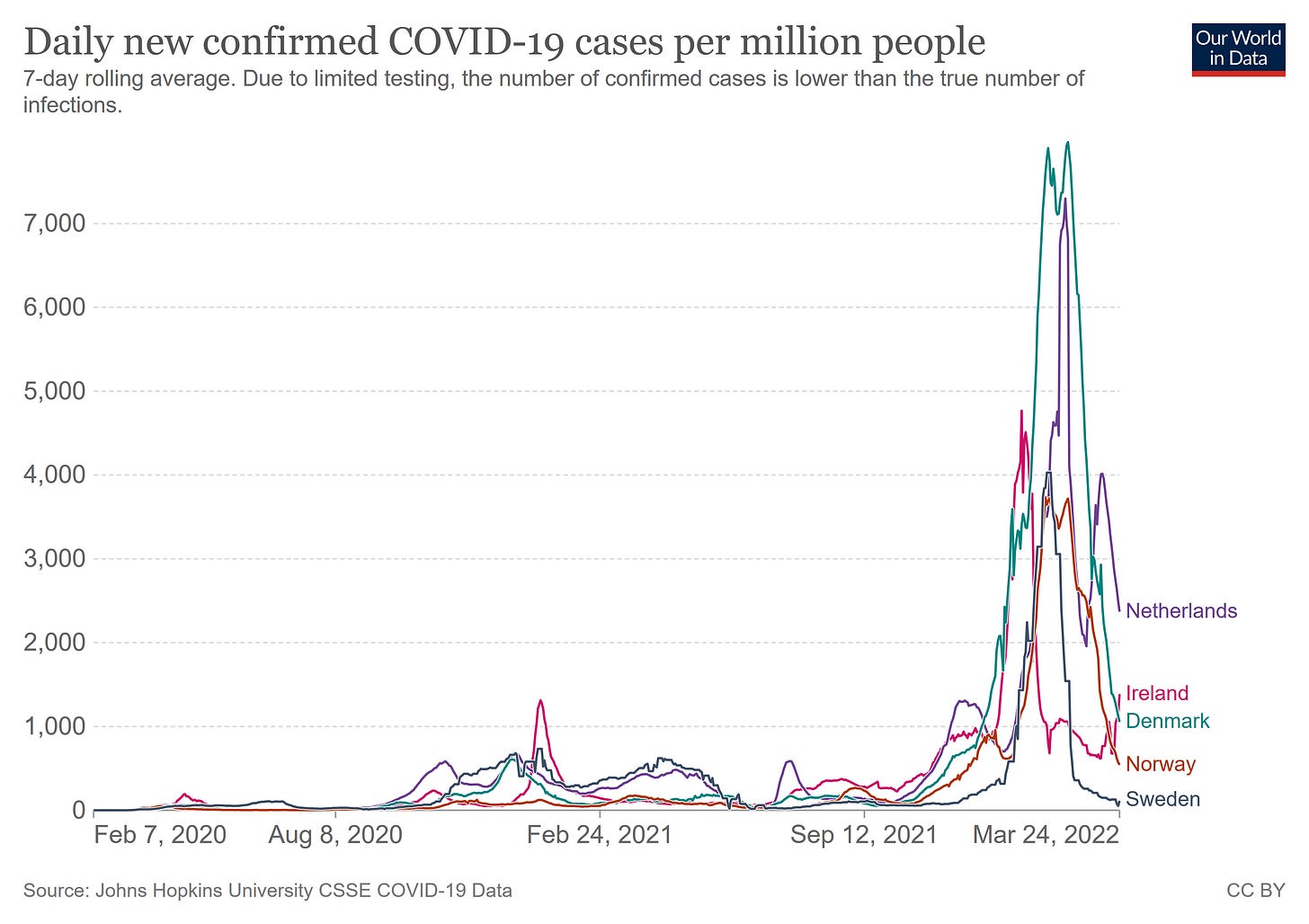
Even Europe presents a mixed picture regarding the BA.2 variant. At least five countries (Netherlands, Ireland, Denmark, Norway, and Sweden) which experienced significant Omicron outbreaks are now showing effective reproduction rates for the virus well below 1 (reproduction rates below 1 mean the disease is diminishing in the population.
The outbreaks were impactful:
But they are also over, as the reproduction rates clearly show:
For these countries at least, COVID-19 is now an “endemic” disease.
Passive Surveillance Worked For The Flu. Let It Work For COVID-19.
What is ironic about the “experts” and their fears is they seem to operate under the genuine belief that, without testing, testing, and more testing, the healthcare infrastructure is powerless to respond to a new COVID-19 surge (or any other disease outbreak, for that matter). Referring back to the AP article, note some of the stated concerns:
—As more people take rapid COVID-19 tests at home, fewer people are getting the gold-standard tests that the government relies on for case counts.
—The Centers for Disease Control and Prevention will soon use fewer labs to look for new variants.
—Health officials are increasingly focusing on hospital admissions, which rise only after a surge has arrived.
The irony of this is that, pre-COVID, hospital visits and admissions was exactly how the nation’s healthcare infrastructure, from the CDC on down to the local hospital, tracked the panopoly of pathogens covered under the rubric “Influenza Like Illness” (which, strictly speaking, includes the SARS-CoV-2 virus).
Moreover, as I discussed two years ago, the reliance on testing and not hospital visits/admissions not only does not work for disease tracking, it has never worked for disease tracking.
Additionally, that assumes that the testing itself is accurate and reliable. As has been tacitly admitted even by CDC Director Rochelle Walensky, the “gold standard” PCR tests the “experts” want to see used more, are neither accurate nor reliable.
What is the surveillance system the CDC has used literally for years pre-COVID? Simply their Weekly U.S. Influenza Surveillance Report. The surveillance report itself provides a wealth of data on the number of influenza tests administered (to symptomatic patients visiting the doctor or in hospital as a diagnostic procedure), as well as the various influenza variants being detected across the nation, plus it also highlights the syndromic surveillance efforts of the U.S. Outpatient Influenza-like Illness Surveillance Network (ILINet):
The U.S. Outpatient Influenza-like Illness Surveillance Network (ILINet) monitors outpatient visits for influenza-like illness [ILI (fever plus cough or sore throat)], not laboratory-confirmed influenza, and will therefore capture respiratory illness visits due to infection with any pathogen that can present with similar symptoms, including influenza, SARS-CoV-2, and RSV. Due to the COVID-19 pandemic, health care-seeking behaviors have changed, and people may be accessing the health care system in alternative settings not captured as a part of ILINet or at a different point in their illness than they might have before the pandemic. Therefore, it is important to evaluate syndromic surveillance data, including that from ILINet, in the context of other sources of surveillance data to obtain a complete and accurate picture of influenza, SARS-CoV-2, and other respiratory virus activity. CDC is tracking the COVID-19 pandemic in a weekly publication called COVID Data Tracker Weekly Review. Information about other respiratory virus activity can be found on CDC’s National Respiratory and Enteric Virus Surveillance System (NREVSS) website.
In the CDC’s weekly archives one can find tables detailing the outpatient visits to ILI providers for ILI symptoms.
Nor does syndromic surveillance rely solely on the CDC. State and local health departments regularly publish influenza reports during the traditional winter months comprising the “cold and flu season”. Texas, Florida, and every other state in the Union releases this information every week, and has been for years. Ditto virtually every city and county health agency (a DuckDuckGo search for “influenza report” plus your city or county should reveal the particular name used for the report covering your area).
As my two-year-old commentary demonstrates, the core of this infrastructure is not new. Obviously, the COVID reporting is new to the pandemic era, but the NREVSS is decades old.
NREVSS was created in the 1980s to monitor seasonal trends in influenza and respiratory syncytial virus (RSV). In 2007, data collection for rhinovirus, enterovirus, and human metapneumovirus began. Influenza specimen information, also reported to NREVSS, is integrated with CDC Influenza Surveillance. On a weekly basis, participating U.S. laboratories from university and community hospitals, selected state and county public health departments, and commercial entities, voluntarily report the total number of tests performed, the method used for detection, and the number of those tests with positive results. Reports include virus antigen detections, isolations by culture, and polymerase chain reaction (PCR) results on a weekly basis.
If the “endemic phase” of a pathogen is that phase where it becomes part of the environmental background, then surely the tools appropriate for that period are the background surveillance tools that are already in place and are proven to function. Tools the CDC and the nation's public health agencies at both the state and local level already have, and used reliably pre-COVID.
If Not BA.2, Then Another Pathogen. But Until It Arrives, Don’t Panic
Human history teaches us one thing about disease: it is going to happen. Perhaps BA.2 will become yet another COVID “surge”, yet even if it does not, it is absolutely certain that, eventually, there will be another disease, another epidemic, and another series of surges. When it comes to infectious disease, this is ever and always the order of things.
The presence of BA.2 is thus not a threat so much as it is an opportunity. It is a chance for the public health infrastructures to distance themselves from the discredited and disproven “testing testing testing” modality and return to the more rational as well as more sustainable modality of syndromic surveillance coupled with laboratory testing when patient symptoms warrant, a modality that already exists and requires no new programs, no new protocols, and, best of all, no new funding (or did I just hit on a reason for the continued Pandemic Panic?).
Mass testing did not make sense two years ago, and it does not make sense today.
Syndromic surveillance did make sense two years ago and it does make sense today. The passive surveillance mechanisms the CDC has built up and refined for decades made sense two years ago and they make sense today.
Instead of Pandemic Panic, how about “Don’t Panic”? Not only is that a more sustainable way to go about daily living, but it is a superior and proven way to approach endemic infectious disease.
BA.2 is endemic. SARS-CoV-2 is endemic. The nation’s healthcare infrastructure needs to respond to them as such, and that means not perpetuating the Pandemic Panic of the past two years.
The “experts” will just need to get used to that.