And...It's Gone: Philly Ends Mask Mandate After Just Ten Days
The (Political) "Science" Just Won't Stop Changing
In an abrupt reversal, the Philadelphia Board of Health voted to rescind the indoor mask mandate a mere 10 days after voting to reimpose it on the city.
"Due to decreasing hospitalizations and a leveling of case counts, the city will move to strongly recommend masks in indoor public spaces as opposed to a mask mandate," a department spokesperson said in a statement late on Thursday. "Given the latest data, the BOH voted to rescind the mandate.”
This is a remarkable instance of reality setting in, given that ten days ago the sentiment on the Board was that a new infection wave was beginning.
New infections in Philadelphia are rising quickly, up 50% from the start of April, prompting the city to step up prevention measures, city Health Commissioner Cheryl Bettigole said at a news briefing. COVID hospitalizations, a lagging metric, remain stable, she said.
"This looks like we may be at the start of a new COVID wave, like Europe just saw," Bettigole said.
In just ten days, the “science" on universal masking did a 180, as the feared wave never showed up.
Much Ado About Nothing?
The magnitude of Philadelphia's nascent infection “wave" is—and has been—debatable. According to the city’s own data, infections are up somewhat among those age 20-34 (orange line).
Yet the infection increase in that age cohort comes amid an increase in testing.
One reason infections are up among 20-34 year olds is because they're looking more.
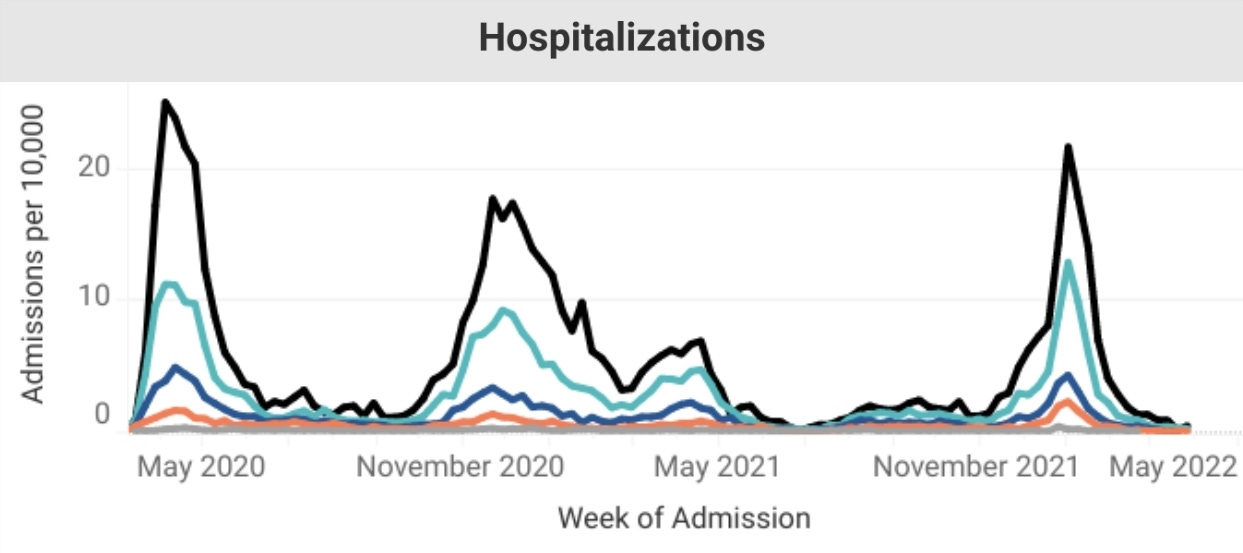
At the same time, there has been no significant rise in hospitalizations.
Deaths from COVID-19 remain low.
Calling the infection increase a “wave" is arguably a demonstrable case of much ado about nothing.
Masks Are Problematic
Mask mandates have been highly controversial since their inception in 2020 for one simple reason: the “science” does not support a masking strategy as an effective mitigation against infectious respiratory diseases, including COVID-19. As I documented in 2020, science has never supported mask mandates.
The decision by Anthony Fauci, et al, to support mask mandates after explicitly denying their utility was a purely political maneuver.
Yet even in this pandemic era, face masking has lacked a solid scientific basis. As statistician Jeffrey H. Anderson observed last year (echoing my observation from 2020), the CDC’s initial stance against mask mandates was the position backed by science and the data.
In truth, the CDC’s, U.K.’s, and WHO’s earlier guidance was much more consistent with the best medical research on masks’ effectiveness in preventing the spread of viruses. That research suggests that Americans’ many months of mask-wearing has likely provided little to no health benefit and might even have been counterproductive in preventing the spread of the novel coronavirus.
At the time of Jeffrey Anderson's article in City Journal, there were fourteen Randomized Controlled Trials (the RCT is considered the “gold standard” of biomedical research). None of them showed masking to be demonstrably beneficial to the general public.
For example, a 2016 study by Professor Chandini Raina MacIntyre of the University of New South Wales found no statistically significant benefit to face masking.
In an intention-to-treat analysis, rates of clinical respiratory illness (relative risk (RR) 0.61, 95% CI 0.18 to 2.13), ILI (RR 0.32, 95% CI 0.03 to 3.13) and laboratory-confirmed viral infections (RR 0.97, 95% CI 0.06 to 15.54) were consistently lower in the mask arm compared with control, although not statistically significant. A post hoc comparison between the mask versus no-mask groups showed a protective effect against clinical respiratory illness, but not against ILI and laboratory-confirmed viral respiratory infections.
A 2010 French study led by Dr. Laetitia Canini found no statistical difference between the intervention and control groups.
We did not show any significant difference in ILI proportion among household contacts between the intervention arm and the control arm.
Lather. Rinse. Repeat. Each of the fourteen Randomized Controlled Trials on the efficacy of masking failed to establish any benefit to the public health strategy.
Lies, Damned Lies, And Bangladesh
The one Randomized Controlled Trial actually cited by the CDC to support its defense of mask mandates is last year's Bangladeshi study.
A large, well-designed cluster-randomized trial in Bangladesh in late 2020 found that surgical or cloth mask distribution, role-modeling, and active mask promotion tripled mask use to 42.3% in intervention villages compared to 13.3% in comparison villages. In villages receiving mask interventions, symptomatic seroprevalence of SARS-CoV-2 was reduced by approximately 9% relative to comparison villages. In villages randomized to receive surgical masks, symptomatic seroprevalence of SARS-CoV-2 was significantly lower (relative reduction 11.1% overall). The results of this study show that even modest increases in community use of masks can effectively reduce symptomatic SARS-CoV-2 infections (COVID-19).
The Bangladeshi study is perhaps the largest study of face mask strategies ever done, encompassing hundreds villages across Bangladesh and hundreds of thousands of Bangladeshis. The scientific media was suitably awed by the size of the study to suggest that the question of masking as an effective mitigation was definitively answered once and for all.
“This really should be the end of the debate,” says Ashley Styczynski, an infectious-disease researcher at Stanford University in California and a co-author of the preprint describing the trial.
Unfortunately, other reviewers quickly realized that the study, though large, was hardly well-designed, and its glowing results for face masking were more due to confirmation bias, wishful thinking, and some very fuzzy math.
Denis Rancourt, a researcher with the Ontario Civil Liberties Association in Canada, found the study to be “fatally flawed".
The cluster-randomized trial study of Abaluck et al. (2021) is fatally flawed, and therefore of no value for informing public health policy, for two main reasons:
The antibody detection was performed using a single commercial FDA emergency-use-authorized (EUA) serology test that is not suitable for the intended application to SARS-CoV-2 in Bangladesh (not calibrated or validated for populations in Bangladesh; undetermined cross-reactivity against broad-array IgM antibodies, malaria, influenza, etc.).
The participants (individual level, family level, village level) in the control and treatment arms were systematically handled in palpably different ways that are linked to factors established to be strongly associated to infection and severity with viral respiratory diseases, in particular, and to individual health in general.
Just the use of an inappropriate serology test is sufficient to disqualify the study from consideration, as a poor testing mechanism to confirm SARS-CoV-2 infection renders the results unreliable.
Yet Abaluck's scientific sins do not stop there. His protocol corrupted the intervention group by repeated interactions and intrusions to manipulate their behavior.
Let me start by stating the obvious, since it seems to have escaped detection by virtually all media and public-relations reviewers (including the folks at Nature): A trial in which the researchers spend significant resources to convince the non-control group to accept or adopt the treatment is not a “randomized” trial, nor is it “controlled”. Rather, it is a trial in which one group is chosen to be intrusively manipulated to receive the treatment, whereas the other group is free from this manipulation. The trial design is not one in which the treatment and control groups are distinguished by the presence or absence of treatment, as the sole systematic difference. In addition, in this case, individuals in both groups are free to adopt the treatment or not, and that choice is anything but random, in both groups. If anything, the study of Abaluck et al. is in-effect merely another comparative study, but with extensive researcher interference.
Statistician William Briggs also found significant flaws with mathematics of the Bangladeshi study. Far from the “significant” results claimed by Abaluck, it turns out for the demonstration of efficacy, reduction in seroprevalence of SARS-CoV-2, the benefit seen in the study was 0.0026%.
The term “statistical noise “ was devised for precisely this type of experimental outcome.
Far from demonstrating efficacy, the Bangladeshi study in truth shows the exact opposite. The study once again shows no significant benefit to a public health strategy of universal masking.
Mark Twain's pithy observation about lies, damned lies, and statistics fits the Bangladeshi study of face masking almost perfectly.
The Science And The Data Don't Change, Just The Politics
Contrary to the endless rationalizations of bureaucrats and the public health “experts”, neither the science nor the data has ever changed, not on face masks nor on any other aspect of the Pandemic Panic Narrative. There has never been a good case to be made for universal masking, either indoors or out. The mask mandates were pure politics in April of 2020 and they are pure politics now.
Bad logic and worse science have been the hallmarks of the Pandemic Panic Narrative from the very beginning. This is the inevitable consequence of the fatal Faucist brew of politics with science--the politics soon prevails while the science suffers. That was the case on April 11, when the Philadelphia Board of Health resurrected the mask mandate, and it is the case now that the Board is reversing itself.
Throughout the Pandemic Panic Narrative, one principle has always remained intact: Real science never changes. Political “science” never stops changing.








Mask mandates have exactly one purpose, which is purely psychological. They serve to remind everyone that there's a "pandemic" and that we should all live in fear.