COVID Cases In Minnesota And Michigan: The Hospital "Surge" That Isn't
Once Again, The Data Contradicts The Narrative
This week the media has been focusing on the rising COVID-19 case numbers in Minnesota and Michigan, and across the Midwest in general, reminding one and all that the virus has not left us (and likely never will).
However, once again the media reporting falls somewhat short of accurately representing the healthcare situation (something I have covered repeatedly since the pandemic began).
Minnesota: The Hospital Are Full…Aren’t They?
On November 17, the Associated Press reported that Minnesota hospitals were being filled with “unvaccinated” COVID patients.
Minnesota has become one of the country’s worst hotspots for new COVID-19 infections. Hospital beds are filling up with unvaccinated people, and staffers are being worn down by the surge. Health Commissioner Jan Malcolm said Tuesday that she’s ready to expand access to booster vaccines to all adults by the end of the week if the federal government doesn’t act first.
Unfortunately for the Associated Press and Minnesota Health Commissioner Jan Malcom, the data hospitals report regularly to the Department of Health and Human Services—and which in turn is presented graphically through Johns Hopkins University, at the state level, the hospitals are not reported as being full, period:
Statewide, inpatient hospital beds in Minnesota are reported at 82% of capacity as of this writing. Minnesota has 1,787 unoccupied hospital beds and 1,522 beds occupied with COVID-19 patients.
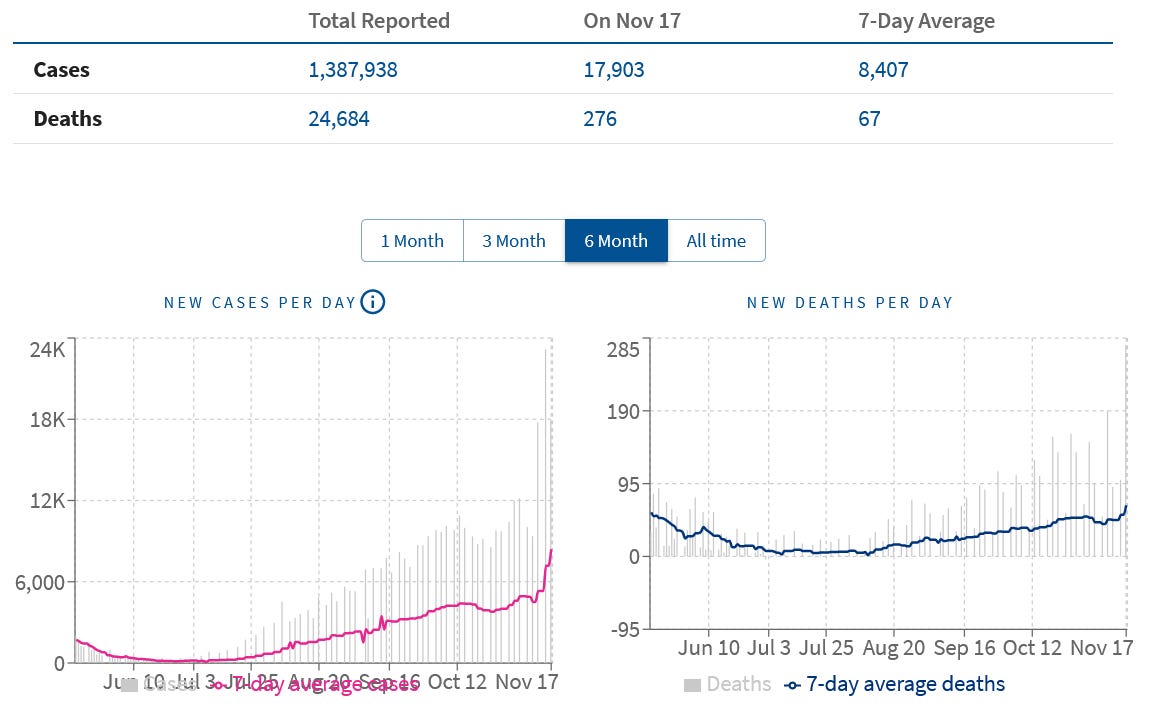
This does not mean there has not been an increase in COVID-19 cases in Minnesota. There unquestionably has been a significant rise in cases and deaths during the past several weeks:
In response to this rise in cases, the Department of Defense is sending medical teams to two of Minnesota’s hospitals, Hennepin County Medical Center and St. Cloud Hospital.
The Department of Defense will send medical teams to two major Minnesota hospitals to relieve doctors and nurses who are swamped by a growing wave of COVID-19 patients, Gov. Tim Walz announced Wednesday.
The teams, each comprising 22 people, will arrive at Hennepin County Medical Center and St. Cloud Hospital next week and begin treating patients immediately, Walz said in a conference call from the Finnish capital of Helsinki. the latest stop on his European trade mission.
However, when we look at the patient data for Hennepin County Medical Center, while the hospital is at or near capacity, we find that COVID patients are not necessarily the cause of the burden.
Note: The hospital-level data lags by two weeks, and the cutoff for these analyses is November 5. However, as the aggregate statewide data provided through Johns Hopkins shows no extraordinary surge at the state level, we may safely presume for now that the hospital level fluctuations follow a similar pattern.
As the chart demonstrates, Hennepin County is truly operating close to inpatient capacity—but there are some important caveats here.
First, Hennepin County’s total supply of inpatient beds is reported to HHS as having declined since the fall of 2020. From an October, 2020 peak of 482 beds, current bed capacity as of November 5 is reported to HHS as being 413—a lost of nearly 69 beds, or 14.5% of the original total supply.
Were those 69 beds still available, Hennepin County Medical Center would have much greater resources for treating patients of all types. As a simple matter of hospital administration, reducing bed capacities during a pandemic is generously described as counter-intuitive (and the rationale for such resource reductions deserves to be part of the public discourse, which currently it is not).
More importantly for the COVID-19 pandemic narrative, however, is the demonstrable fact that, while COVID-19 patients in hospital are on the rise, the increase relative to available beds and total patient population at Hennepin County is significantlyn more gradual than a depiction of a “surge” brings to mind. For the week of November 5, Hennepin County treated a 7-day average of 19.3 COVID-19 patients, while a total of 330 inpatient beds were occupied for all illnesses and conditions.
To be sure, even two weeks ago Hennepin County was operating at 93% capacity (capacity being reported as being 354.4), and even a small increase in patient population would be sufficient to fill the hospital to 100% of its reported capacity.
However, to ascribe the totality of the hospital’s patient burden to COVID-19 is disingenuous at best, and deceitful at worst. It certainly is not accurate to say that COVID-19 patients are “filling up” the hospital. The non-COVID causes of inpatient care are at least as relevant in this regard as the COVID cases.
When we look at the HHS data for St Cloud Hospital, we see a similar pattern:
While COVID-19 patients are on the rise at St. Cloud, as of November 5 there has been no extraordinary patient surge. The hospital is very nearly full, but mostly with non-COVID-19 patients.
Again, we see a noticeable drop in the total number of available beds, from a pre-pandemic level of 500 to 427 as of November 5—a loss of 73 beds, or 14.6% of capacity.
Given the current saturation condition of St. Cloud Hospital, one can readily see that if the full 500 beds from the pre-pandemic era were being utilized, the additional resources would be extremely helpful in the current situation.
Why were those beds eliminated? The HHS data does not say.
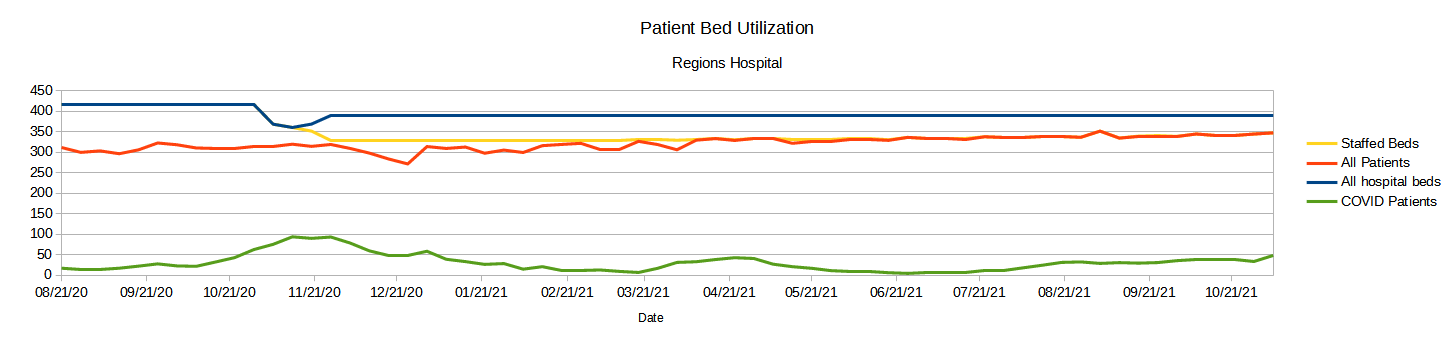
Moreover, when we examine other Minnesota hospitals, such as Regions Hospital in Saint Paul, the same pattern emerges.
Regions Hospital is running at or very near 100% of staffed hospital beds, although not at 100% of all hospital beds, but the patient population is mainly non-COVID patients. At Regions Hospital just as at Hennepin and St. Cloud, staffed bed capacity has declined since the start of the COVID-19 pandemic, and remains significantly less than the total available beds at the hospital.
It also bears mentioning that the rise in reported COVID-19 hospitalizations is not tracking the rise in COVID-19 cases. While cases are up significantly, hospitalizations are increasing much less dramatically.
Michigan: Lots Of Patients. Even More Hospital Beds
Michigan is the other state labeled in the media as a “hot spot” for COVID-19, and, according to the media narrative, whose hospitals are being filled with COVID-19 cases.
Henry Ford Health and Spectrum Health across the state in Grand Rapids, Michigan, together reported 700 COVID-19 patients in their hospitals, the majority of whom were not vaccinated. Positive test rates were running above 20%.
Again, we must acknowledge the real rise in COVID-19 cases in the state.
However, we again must note the existence statewide of available patient bed capacity.
As of this writing, Michigan reports inpatient beds at 85% of capacity, with 3,461 available beds, and 3,357 COVID-19 patients.
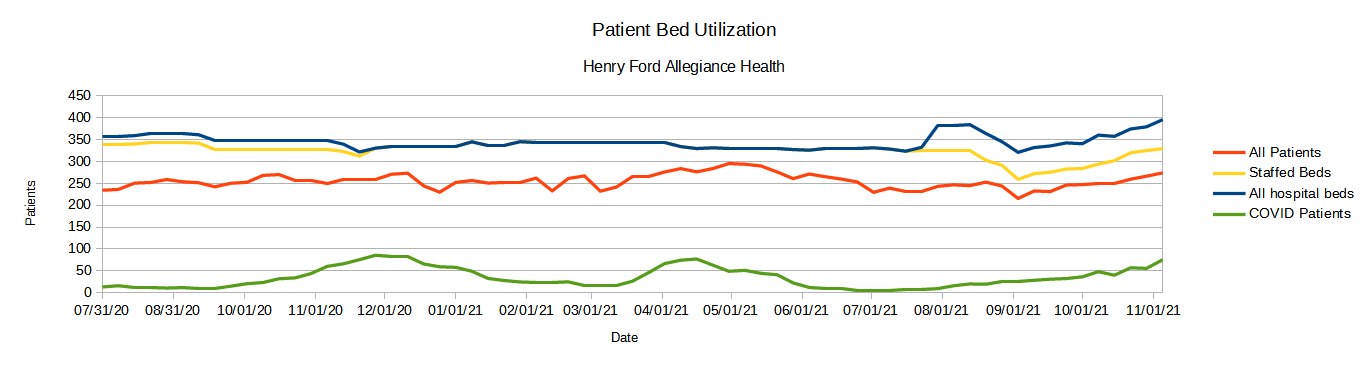
Moreover, when we drill into individual hospitals within the Henry Ford and Spectrum Health hospital systems, we again see that the focus on COVID-19 patients is exaggerated—there are far more non-COVID patients.
At Henry Ford Allegiance Hospital in Jackson, Michigan, for example, as of November 5, the hospital was at 83.2% of staffed inpatient capacity, with 76 COVID-19 patients.
While COVID-19 hospitalizations are rising at this facility, the overwhelming majority of patients are not COVID-19 related. As in Minnesota, we also see that staffed patient beds are not 100% of all available beds at the present time.
Spectrum Health’s Butterworth Campus in Grand Rapids, Michigan, tells a similar tale, operating at 93.9% of capacity as of November 5, with 159 COVID-19 patients.
While the number of COVID-19 patients is rising here as well, it is still very much the minority of the hospital’s patient population.
All Patients Matter
Hospitals exist to serve the entirety of a patient population. The mission of healthcare is to attend to all who are sick and in need of treatment. To single out a particular patient demographic and claim that demographic is overwhelming hospitals, when that demographic is in every instance a minority of patients, is both disingenuous and discriminatory.
To ignore the total capacity of all the hospitals within a state is both discriminatory and dishonest.
COVID-19 cases in Minnesota and Michigan are rising, and some of their hospitals are running at or near capacity. Both of these statements are unambiguously true. The inference that the one is directly and solely responsible for the other is simply not supportable when viewed against the totality of the data. People still get sick with more than just COVID-19, and still require treatment for more ailments than COVID-19.
When addressing the very real resource challenges any state’s healthcare system faces, it is imperative the needs and requirements of all patients be realistically appraised and considered.
We need to always remember that all patients really do matter—both COVID and non-COVID, both inoculated and non-inoculated.










Great article!!!!