The Latest Japanese Study On Omicron BA.2 Is The Triumph Of Theory Over Reality
Lab Research Must Always Be Sanity Checked Against The Real World
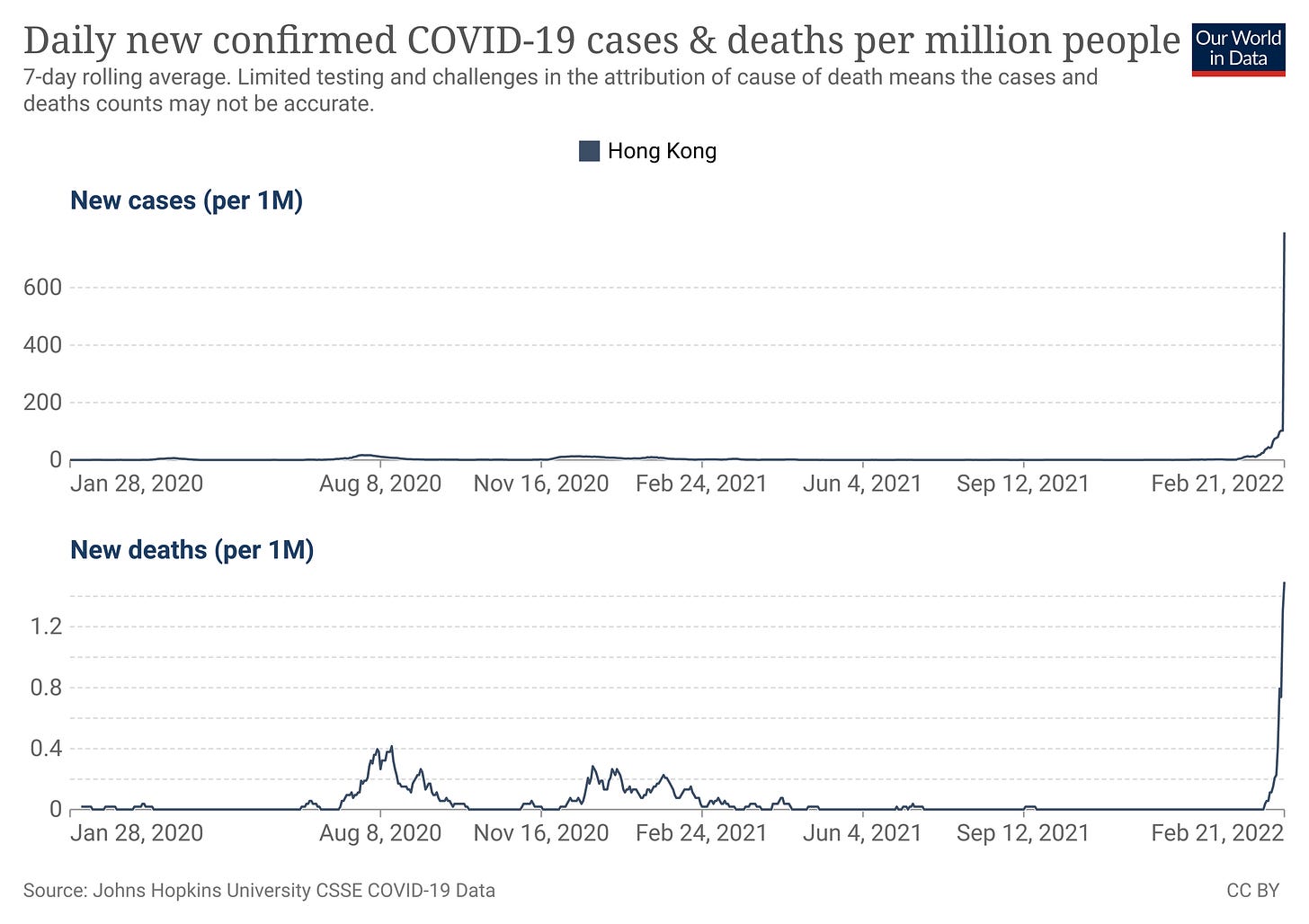
With COVID-19 on the wane almost everywhere, despite fresh spikes of cases and deaths such as is happening in Hong Kong, it is especially important now to appraise new research into the disease with a critical, and even a skeptical, eye.
It is with such a perspective that we consider the latest research into COVID-19, a preprint study coming out of Japan on the Omicron subvariant BA.2.
A Combination Of Math And Lab Research
The first thing to understand about this study is that it is a combination of statistical math and lab research.
Soon after the emergence and global spread of a new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron lineage, BA.1 (ref1, 2), another Omicron lineage, BA.2, has initiated outcompeting BA.1. Statistical analysis shows that the effective reproduction number of BA.2 is 1.4-fold higher than that of BA.1. Neutralisation experiments show that the vaccine-induced humoral immunity fails to function against BA.2 like BA.1, and notably, the antigenicity of BA.2 is different from BA.1. Cell culture experiments show that BA.2 is more replicative in human nasal epithelial cells and more fusogenic than BA.1. Furthermore, infection experiments using hamsters show that BA.2 is more pathogenic than BA.1. Our multiscale investigations suggest that the risk of BA.2 for global health is potentially higher than that of BA.1.
While this provenance for the study should not be taken as a disparagement, it nevertheless establishes the study as largely conceptual regarding the public health rather than an empirical assessment of actual disease.
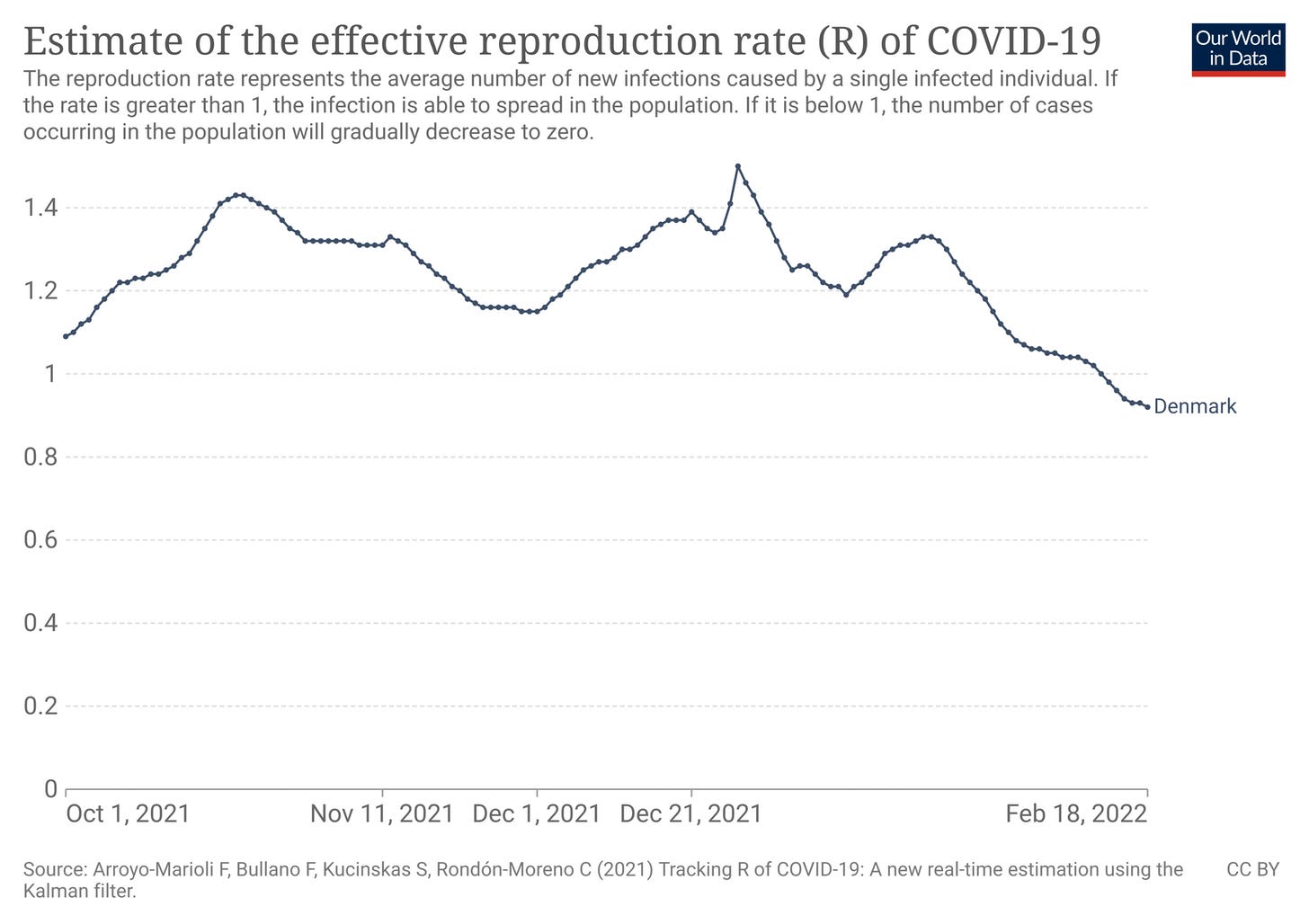
Case in point: the assertion that BA.2's effective reproduction number is 1.4 times greater than BA.1 overlooks the fact that the effective reproduction number is time sensitive.
Explanation of the time course of an epidemic can be partly achieved by estimating the effective reproduction number, R(t), defined as the actual average number of secondary cases per primary case at calendar time t (for t >0). R(t) shows time-dependent variation due to the decline in susceptible individuals (intrinsic factors) and the implementation of control measures (extrinsic factors). If R(t)<1, it suggests that the epidemic is in decline and may be regarded as being under control at time t (vice versa, if R(t)>1).
Thus, even though the number for BA.2 is greater than for BA.1, that increased value is still time sensitive and still represents declining cases when less than one. The BA.2 number could be ten times that of BA.1 and this would still be true.
A Mountain Out Of A Molehill
The study grounds itself—or attempts to ground itself—in the UK Health Security Agency's Technical Briefing Number 35 on the SARS-CoV-2 virus. In particular, it references that briefing to support its claim that BA.2 is outcompeting BA.1.
As of February 2022, another variant of Omicron, the BA.2 lineage, has detected in multiple countries such as Denmark and UK. Notably, BA.2 has initiated outcompeting BA.1, suggesting that BA.2 is more transmissible than BA.1.
Does the briefing support that claim? Not necessarily.
BA.2 does show a higher growth rate than BA.1.
BA.2 has an increased growth rate compared to BA.1 in all regions of England where there are sufficient cases present to make an assessment. Whilst growth rates can be overestimates early in the emergence of a variant, the apparent growth advantage is currently substantial.
Within households, BA.2 shows a greater secondary attack rate than BA.1.
Analysis from routine contact tracing data indicated higher secondary attack rates amongst contacts of BA.2 cases in households (13.4%; 95% CI: 10.7%-16.8%) than those for contacts of other Omicron cases (10.3%; 95% CI: 10.1%-10.4%) in the period 27 December 2021 to 11 January 2022. These secondary attack rates are not adjusted for vaccination status and reflect overall growth advantage rather than transmissibility
However, the briefing also shows that BA.2 cases are thus far only marginally higher than BA.1 cases.
Moreover, an overview of the Pangolin lineage for viral samples submitted for genomic sequencing shows BA.1 still has much greater prevalence than BA.2
The assessment that BA.2 is outcompeting BA.1 is, at this time, somewhat premature.
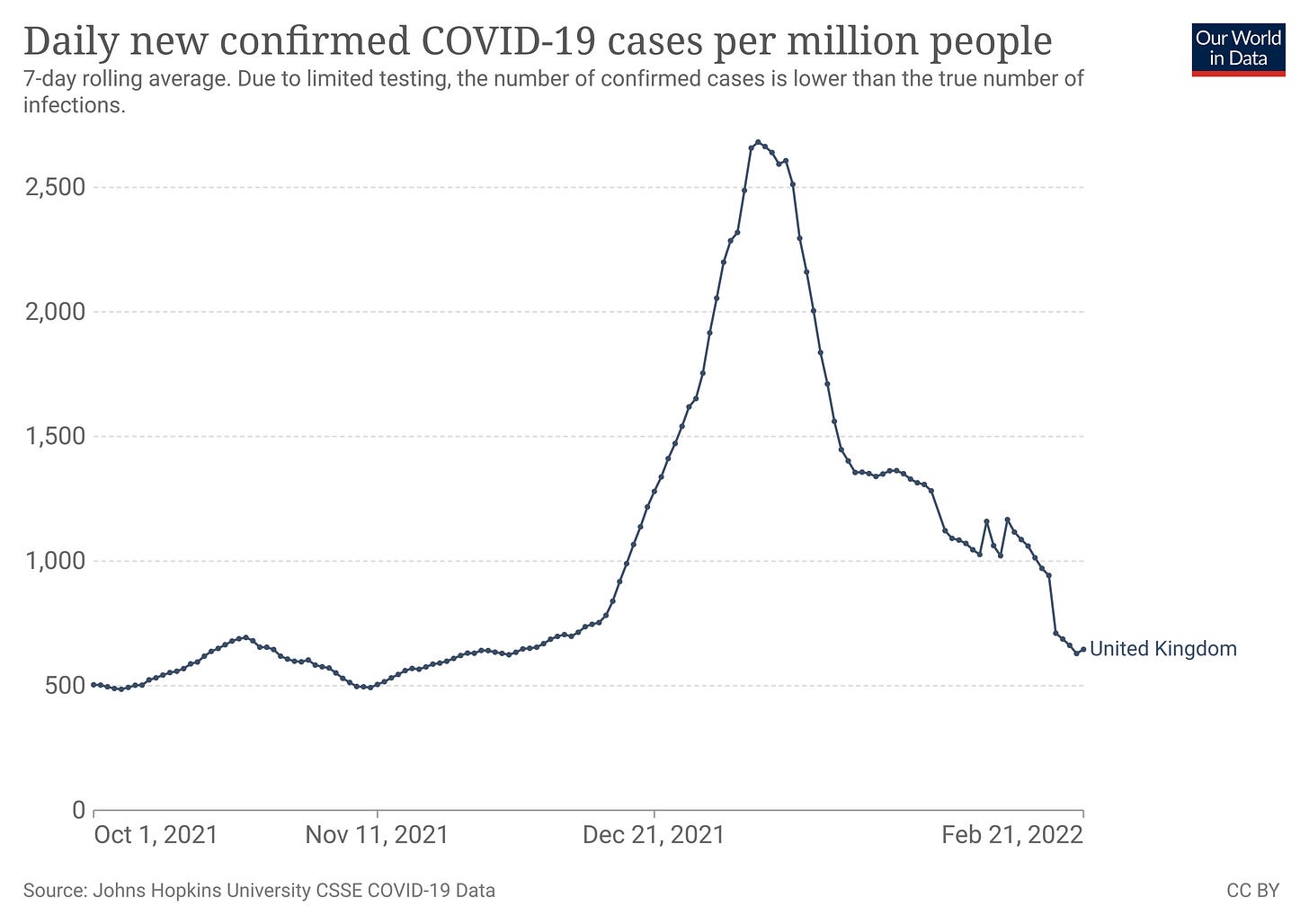
Even so, the empirical backdrop in the UK is that COVID-19 cases have been declining since the new year. BA.2 outcompeting BA.1 at this juncture means only that it is fading more slowly than BA.1.
It should also be noted that Omicron is not the dominant variant in the UK at this time, at least among hospital ICU admissions.
Whatever the infection risks of Omicron may be, whether BA.1 or BA.2, Omicron is not what is sending Brits to the hospital—thus making fears about BA.2's greater infectivity the epitome of a mountain made out of the proverbial molehill.
Tap Dancing Around The Failure Of Big Pharma's “Vaccines”
As is commonplace in the Faucist paradigm of COVID-19 research, the study tap dances around the reality that the Big Pharma “vaccines" are ineffective, especially against Omicron.
Consistent with recent studies, BA.1 is highly resistant to the antisera elicited by mRNA-1273 and ChAdOx1 vaccines (Fig. 2b,c). Similar to BA.1, BA.2 was also highly resistant to the vaccine-induced antisera (Fig. 2b,c). Also, BA.2 was almost completely resistant to two therapeutic monoclonal antibodies, Casirivimab and Imdevimab, and was 35-fold more resistant to another therapeutic antibody, Sotrovimab, when compared to the ancestral D614G-bearing B.1.1 virus (Fig. 2d).
This, of course, confirms what is already known, that Omicron is largely untouched by the “vaccines”, which were never effective in the first place.
Additionally, the poor showing of monoclonal antibody therapies should surprise no one. Casirivimab and Imdevimab were both developed early in the pandemic, against the original SARS-COV-2 virus. Omicron was first found noteworthy because of the high number of mutations from the original virus. As both the Big Pharma “vaccines" and the main monoclonal antibodies were developed against the same spike protein target, which target is greatly shifted in Omicron, there should be no great surprise that, as the “vaccines" are ineffective, so too are the main monoclonal antibody therapies, and for the same reason: both are shooting at the same wrong target.
Understanding Methods: Vitro And In Vivo Experiments. No Patients.
To properly appreciate the scope of this study, one must recognize that no patients were directly involved. Most of research was done in vitro using a variety of cell cultures. The effects of BA.1 and BA.2 viruses on live tissues were studied by infecting the lungs of hand then harvesting those organs for microscopic evaluation.
Human patients did contribute their convalescent blood sera so researchers could evaluate the effectiveness of COVID-19 antibodies generated both by the “vaccines" and by COVID-19 infection. Beyond this, no patients were involved.
This should not be seen as a flaw of the study. This is a study of the SARS-CoV-2 virus, not the COVID-19 disease that it causes. The BA.2 subvariant has a number of mutations which differentiate it even from BA.1 (one conclusion the authors reach is that BA.2 is worthy of its own Greek letter and designation as a stand alone “Variant of Concern”).
What arguably is a weakness of the study is the generation and use in the in vitro research of “chimeric" recombinant SARS-CoV-2 virions rather than actual whole BA.1 and BA.2 viruses.
To investigate the virological characteristics of BA.2, we generated chimeric recombinant SARS-CoV-2 that expresses GFP and harbours the S gene of ancestral B.1.1, Delta, BA.1 and BA.2 by reverse genetics (Extended Data Fig. 4).
Such a technique allows for the impact of specific genes, mutations, and proteins to be the exclusive focus of study, but the tradeoff is limited extrapolation of the results to real world virus behavior. A recombinant SARS-CoV-2 virus might be an excellent means of investigating key mutations of a SARS-CoV-2 variant, but such a structure is by definition not a variant found in the real world. Recombinant SARS-CoV-2 virus which encodes specific BA.2 characteristics is not actual BA.2 virus, and while such a research method is necessary to study specific characteristics and their potential behaviors, only actual BA.2 virus can demonstrate actual behaviors.
Theory vs Reality
Albert Einstein once rather pithily observed that “in theory, theory and reality are the same; in reality, theory and reality are different.” We do well to heed Albert Einstein when contemplating lab studies such as this one.
The results are as they are, but, as they are, being partially the results of studying pseudoviruses, they are very much in the realm of theory and not reality.
This is not to say the results are fictional, but that they present potentials and not actuals. The study shows that BA.2 could pose a greater threat than BA.1, all else being equal. The study shows that BA.2 could pose a reinfection threat even to those who have already been infected by the BA.1 subvariant. The study arguably shows that BA.2 is more a distinct variant rather than just an Omicron subvariant.
However, laboratory results cannot show a rising public health threat from BA.2, nor indeed any pathogen. Laboratory results alone cannot justify calling the BA.2 Omicron subvariant a new Variant of Concern, as the study's authors suggest should be done. Only the empirical case data, mortality data, and hospitalization data can do that. When empirical data of rising cases, hospitalizations, and mortality is absent, there is simply no actual concern to be had, at least from a public health perspective.
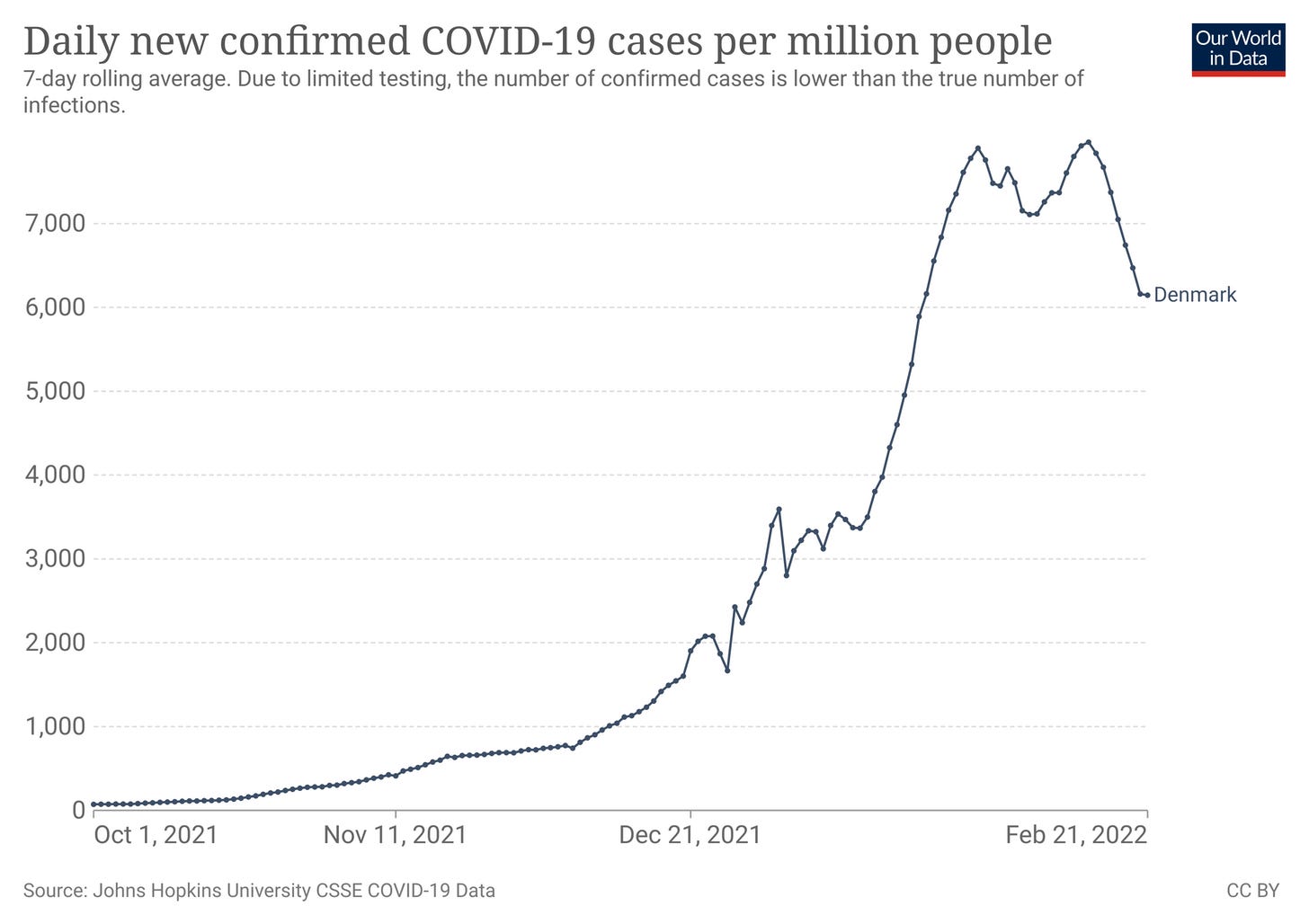
When Denmark's cases are declining…
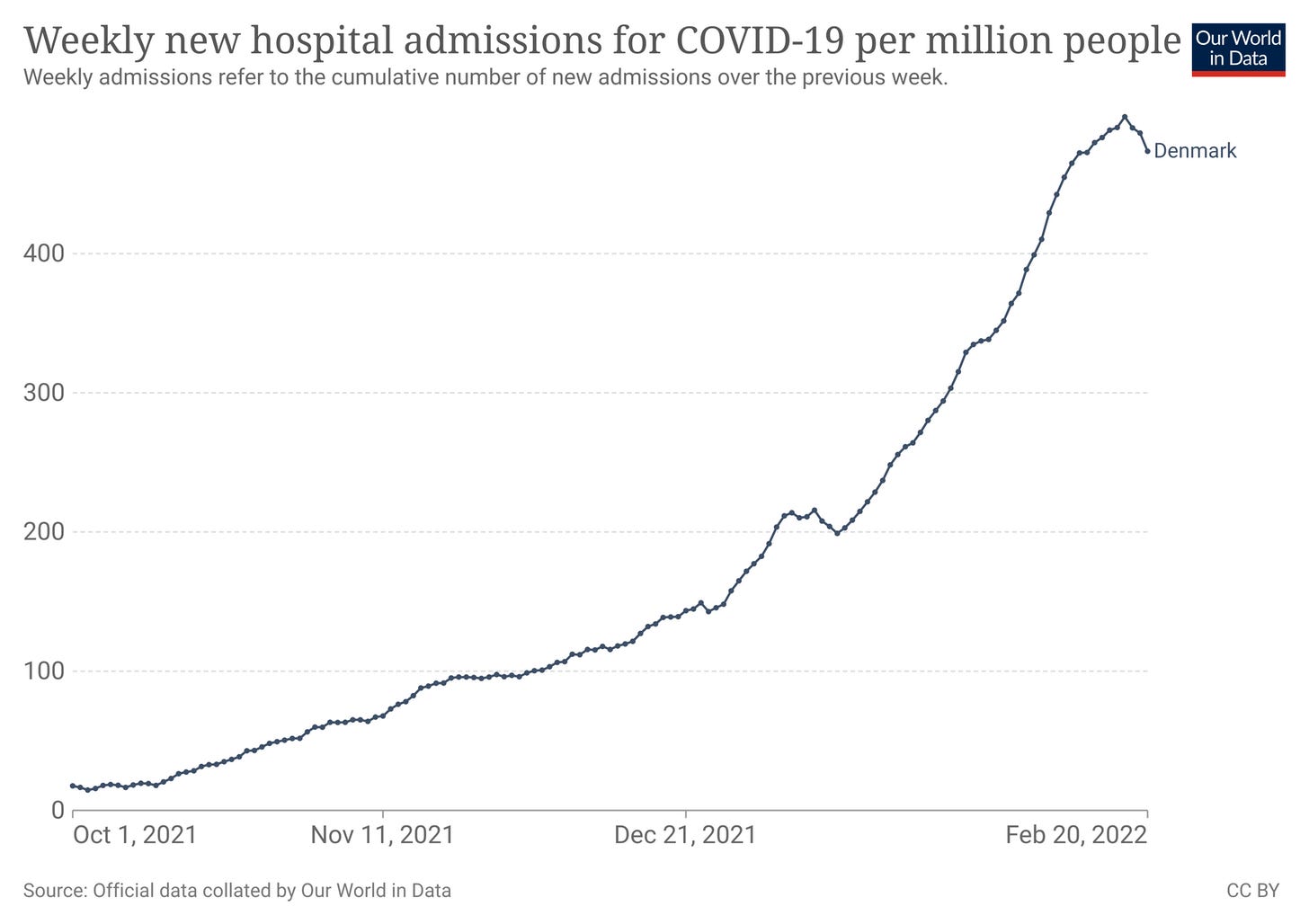
…when Denmark's hospital admissions are declining…
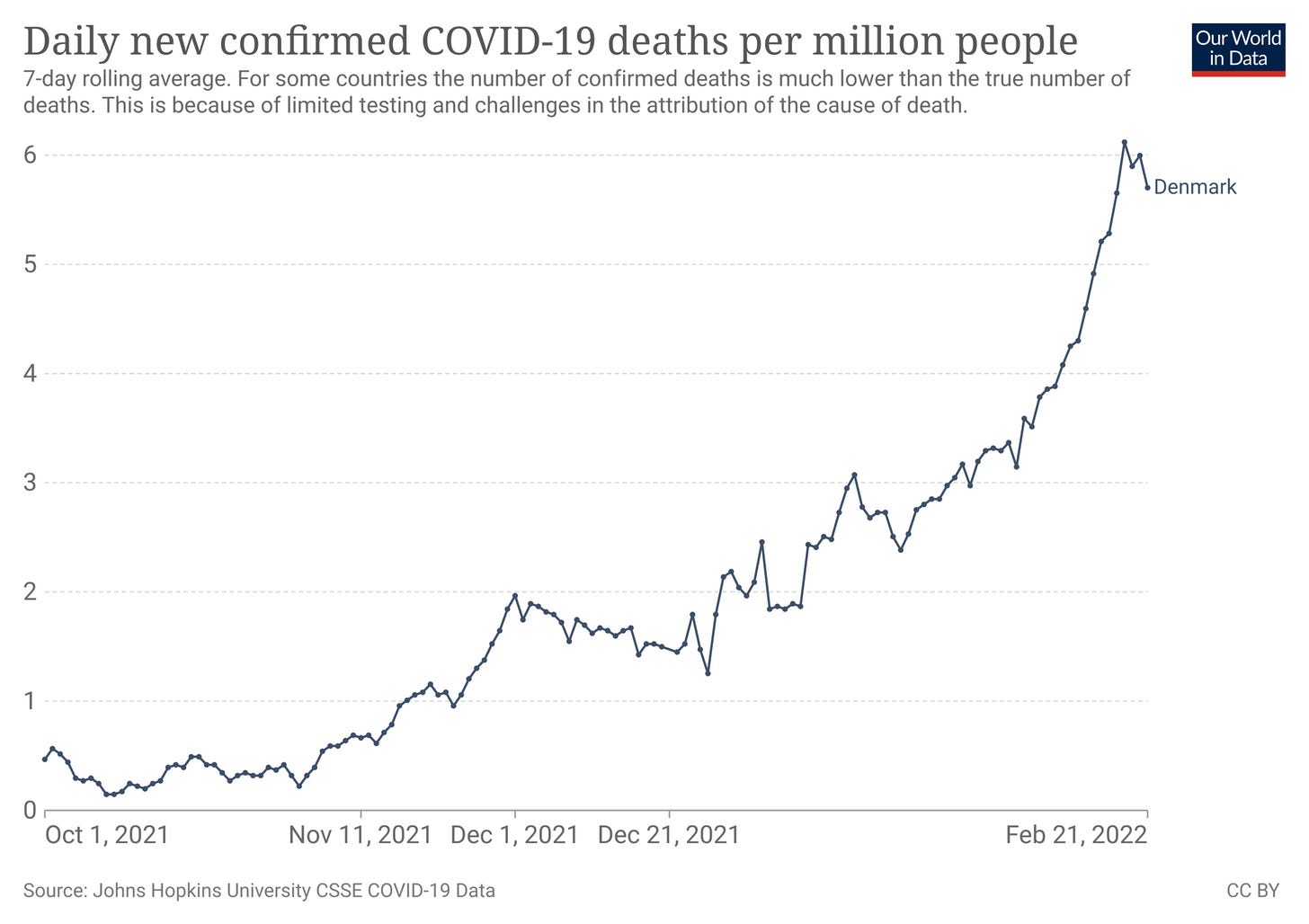
…when Denmark's mortality stats are declining…
…when Denmark's effective reproduction number for COVID-19 is below 1 and dropping…
…there simply is no basis for public health alarm. While this does not rule out a future basis, to raise an alarm over BA.2 without clear empirical evidence is to respond to a crisis that by definition does not yet exist, and may never exist.
The empirical data categorically shows a declining public health threat, not a rising one. Unless and until these empirical trends reverse, concerns about any greater infectiousness if Omicron BA.2 over BA.1 are largely moot.
While a virological understanding of the BA.2 virus, or any SARS-CoV-2 virus, requires research in the realm of theory, public health is indisputably in the realm of reality. We do well not to conflate the two.