Vitamin D: The Real "Magic Bullet" Against COVID-19?
More Effective Than The Vaccines? Arguably, Yes
As I noted the other day, the clinical research shows that COVID-19 is truly a “pandemic of the vitamin D deficient.”
Yet that trite and clichéd formulation overlooks a long-ignored clinical reality: Vitamin D is potentially a superior mitigation than the much ballyhooed “vaccines”, and without the concerns over myocarditis and pericarditis, as well as the many other catastrophic side effects and adverse events arising from the vaccines. Not only are the vaccines not a “magic bullet” against the SARS-CoV-2 virus, but, by comparison, vitamin D makes a pretty good claim on that title.
The Latest Israeli Study
We can begin examining the question of vitamin D's efficacy against COVID-19 by delving into the latest Israeli study to appear in the peer reviewed literature.
This retrospective study examined COVID-19 patients admitted to Galilee Medical Center in Nahariya, Israel, between 7 April 2020 and 4 February 2021. This time frame is important as it is generally before widespread availability of the vaccines. We may safely interrogate the clinical data without the vaccines intruding on the data set.
A total of 1176 patients were admitted to GMC in the study interval, and of those, 253 had measurements of vitamin D in the patient history. The mean age of the 253 patients was 63.3, and the patients were 109 male and 144 female.
Of the 253 patients with vitamin D measurements in the patient history, the overwhelming majority of patients had vitamin D deficiency, defined as <20ng/mL. This was true across all age brackets and in both sexes.
A lower vitamin D status was more common in patients with the severe or critical disease (<20 ng/mL [87.4%]) than in individuals with mild or moderate disease (<20 ng/mL [34.3%] p < 0.001). Patients with vitamin D deficiency (<20 ng/mL) were 14 times more likely to have severe or critical disease than patients with 25(OH)D ≥40 ng/mL (odds ratio [OR], 14; 95% confidence interval [CI], 4 to 51; p < 0.001).
Another significant data point: 34 patients with vitamin D deficiency died while in hospital, versus only 2 with high-normal vitamin D levels (≥40ng/mL).
The vitamin D deficient cohort also displayed much higher incidence of comorbidities than the high-normal cohort.
To say that vitamin D levels are significant to COVID-19 patient outcomes is something of an understatement. When 17 times as many vitamin D deficient patients die as high-normal patients, vitamin D quite plainly occupies a central role in patient outcomes. That is the unambiguous conclusion to be drawn from this study.
One Study Backed By Many Studies
While we should always be leery of reading too much into any single study, this vitamin D study is backed up by a number of other studies that show clear evidence of vitamin D efficacy both in treatment and in prophylaxis. The ongoing meta study of COVID-19 research papers by the @CovidAnalysis research team confirms this many times over.
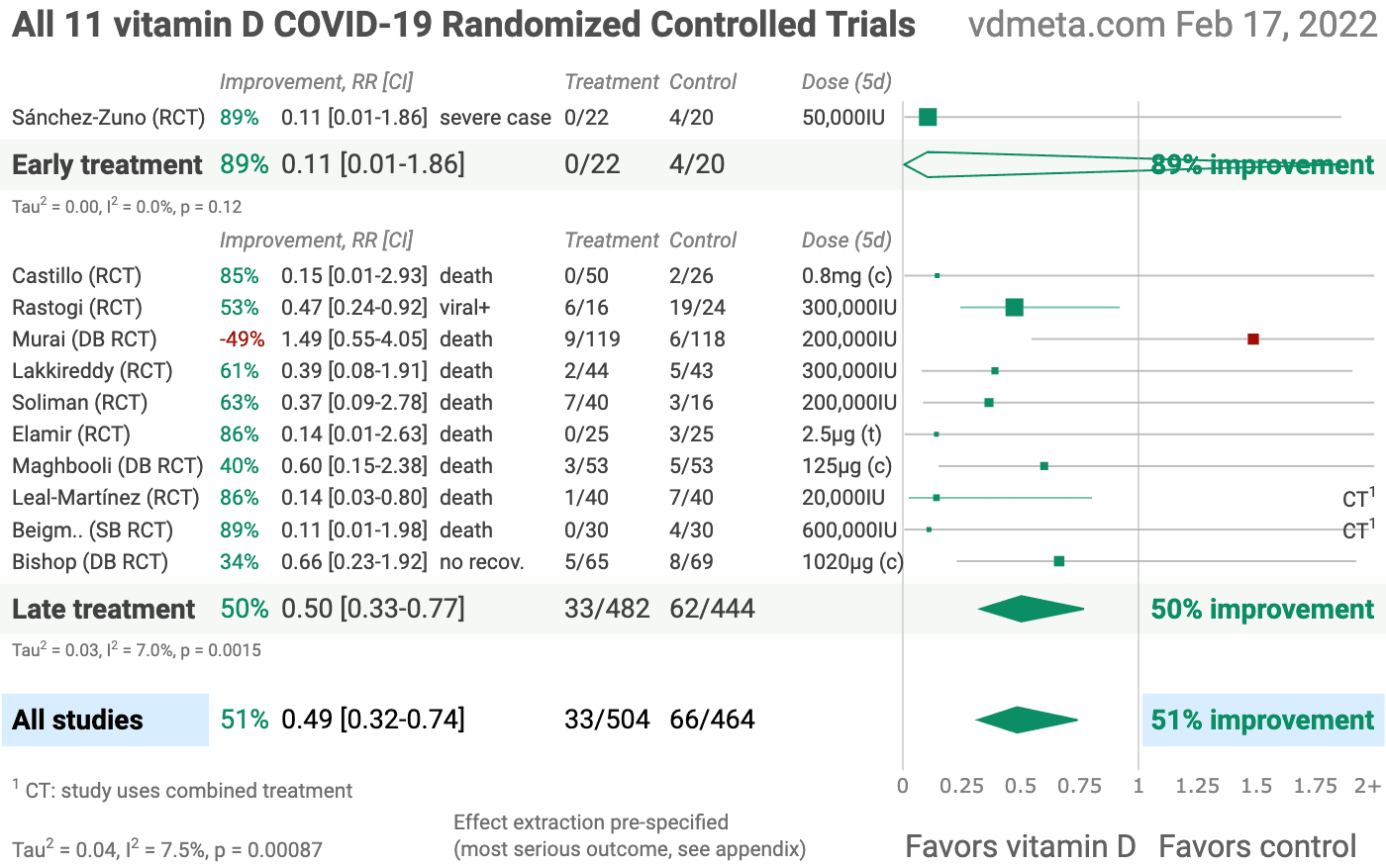
The @CovidAnalysis research team has analyzed, as of this writing, 11 Randomized Controlled Trials which show vitamin D is on average 51% effective in combating COVID-19.
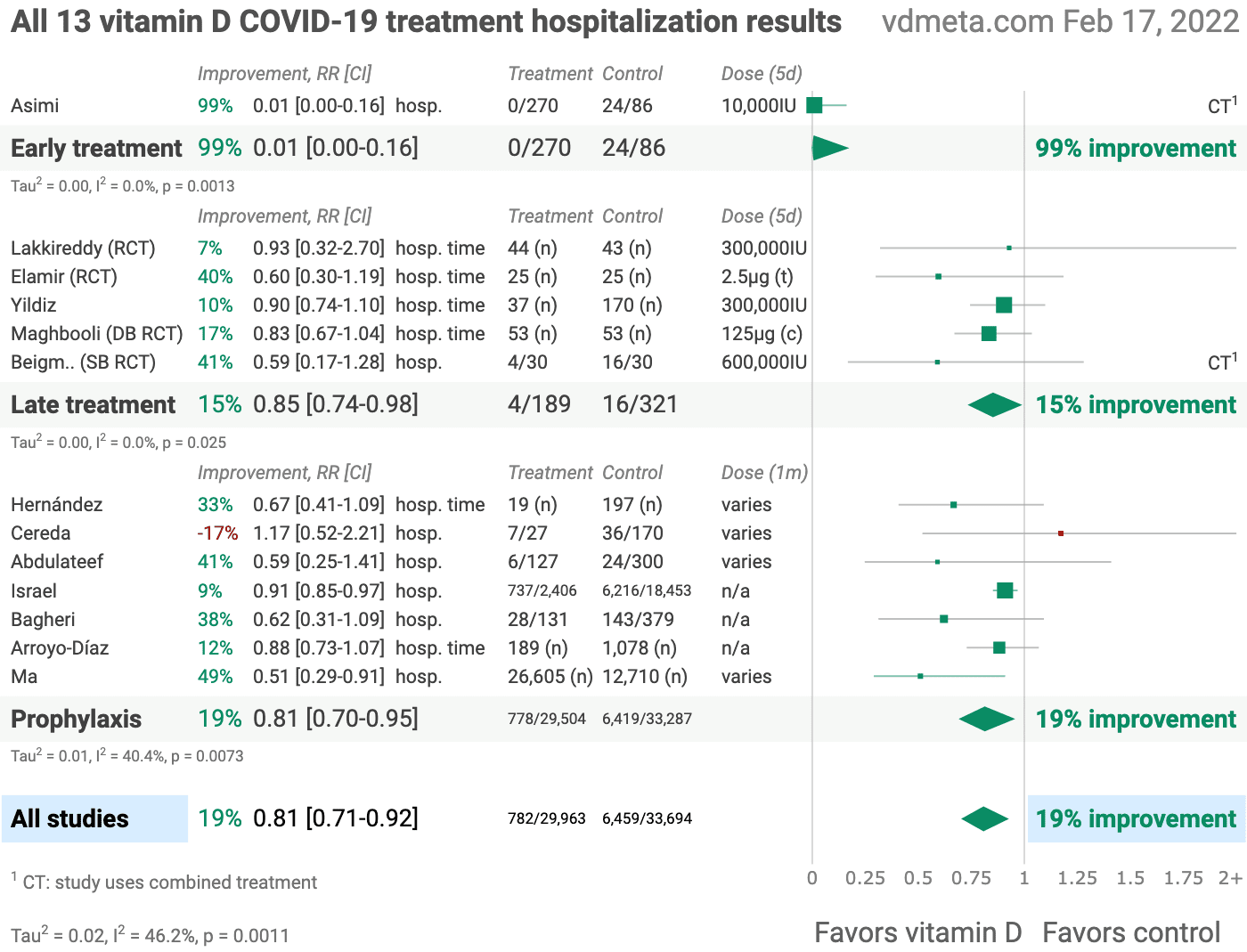
@CovidAnalysis has analyzed, as of this writing, 13 studies showing vitamin D therapy is on average 19% effective in improving hospitalization outcomes. Note that the one early treatment study showed a 99% improvement in COVID hospitalizations.
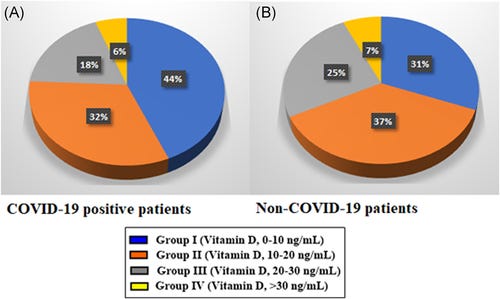
One study published in January, 2021 (again predating general vaccine availability) deserves especial attention. This study, performed in Turkey, also showed vitamin D deficiency playing a significant role in COVID-19 cases and severity.
In the present single-centered retrospective cohort study, vitamin D deficiency was found to be associated with a higher COVID-19 risk. The COVID-19-positive individuals with sufficient vitamin D levels had significantly lower blood levels of D-dimer, inflammatory marker CRP, reduced frequencies of ground-glass opacity appearance in chest CT scans and shorter hospital stays. The findings of the study indicated the need for randomized studies to determine whether the vitamin D level could affect COVID-19 risk.
Meta-analysis of the study encapsulates the observed benefits of vitamin D in COVID-19 outcomes:
risk of severe case, 89.3% lower, RR 0.11, p < 0.001, high D levels 13, low D levels 99, ratio of the mean number of affected lung segments, >30ng/ml vs. <=10ng/mL.
hospitalization time, 87.1% lower, relative time 0.13, p < 0.001, high D levels 13, low D levels 99, >30ng/ml vs. <=10ng/mL.
risk of case, 24.2% lower, RR 0.76, p = 0.18, high D levels 13 of 31 (41.9%), low D levels 99 of 179 (55.3%), NNT 7.5, >30ng/ml vs. <=10ng/mL.
This Demir study also took the step of examining non-COVID patients and reviewing their vitamin D levels. As with the comorbidities in the Dror study with which I began, low vitamin D in this study correlates to general poor health, and not just poor COVID-19 outcomes.
For comparison purposes, 1200 patients who applied to Tokat State Hospital for reasons other than COVID-19 in November 1, 2019–November 1, 2020 period were screened for the availability of their vitamin D measurements, and 260 such patients were identified. Eighty of them (30.76%) (average age, 46.50 ± 2.21 years [range, 20–75 years] and 62.5% women) had vitamin D levels below 10 ng/ml (mean, 6.52 ± 0.19) while 96 patients (36.92%) (average age, 42.19 ± 1.75 years [range, 18–75 years] and 65.62% women) had vitamin D between 10 and 20 ng/ml (mean, 13.51 ± 0.40), 66 patients (25.38%) (average age, 44.36 ± 3.02 years [range, 22–73 years] and 46.96% women) between 20 and 30 ng/ml (mean, 22.72 ± 0.58) and 18 patients (6.92%) (average age, 43.75 ± 4.91 years [range, 26–77 years] and 61.11% women) between 30 and 40 ng/ml (mean, 37.49 ± 1.20). Thus, the vitamin D level was below 30 ng/ml in 93.07% (average age, 44.63 ± 1.30 age [range, 18–75 years] and 59.50% women) of non-COVID-19 patients (Figure 1, Table 2).
These findings also point to one extremely important reason why vitamin D matters in COVID-19 outcomes: inadequate vitamin D levels are broadly correlated with poor health and a weakened ability to fend off infectious respiratory disease in general.
The Data Is Not New
We should also recognize that the importance of vitamin D in immunological health has been noted in the clinical literature going back to at least 1987.
Also, a Randomized Controlled Trial conducted during the winter of 2008-2009 among school age children found vitamin D supplementation significantly reduced influenza infection in the trial group.
Influenza A occurred in 18 of 167 (10.8%) children in the vitamin D3 group compared with 31 of 167 (18.6%) children in the placebo group [relative risk (RR), 0.58; 95% CI: 0.34, 0.99; P = 0.04]. The reduction in influenza A was more prominent in children who had not been taking other vitamin D supplements (RR: 0.36; 95% CI: 0.17, 0.79; P = 0.006) and who started nursery school after age 3 y (RR: 0.36; 95% CI: 0.17, 0.78; P = 0.005). In children with a previous diagnosis of asthma, asthma attacks as a secondary outcome occurred in 2 children receiving vitamin D3 compared with 12 children receiving placebo (RR: 0.17; 95% CI: 0.04, 0.73; P = 0.006).
A 2017 meta-analysis of 25 Randomized Controlled Trials reached a similar conclusion:
Vitamin D supplementation was safe and it protected against acute respiratory tract infection overall. Patients who were very vitamin D deficient and those not receiving bolus doses experienced the most benefit.
It is no exaggeration to say that the evidence of vitamin D's efficacy against infectious respiratory disease, including COVID-19, is voluminous and unambiguous. Vitamin D reduces the risk of severe COVID-19, and more broadly of infectious respiratory disease, by sstrengthening the immune system and improving overall health.
Moreover, if a majority of patients are vitamin D deficient, vitamin D supplementation, which corrects the deficiency, should be expected to show beneficial effects even in treatment, not just in prophylaxis. The clinical data shows exactly this.
The “Experts” And The Media Ignore Vitamin D, Hype The Vaccines Instead
Amazingly, the veritable mountain of evidence supporting vitamin D both aa therapeutic and a prophylactic has been almost completely ignored by both public health “experts” and the mainstream media.
Shortly after the Dror study was submitted to PLoS ONE for peer review, on June 27, 2021, CDC Director Rochelle Walensky began talking about the rising “Delta” wave as a “pandemic of the unvaccinated.”
"There is a clear message that is coming through: This is becoming a pandemic of the unvaccinated," Dr. Rochelle Walensky, the CDC's director, said at a Friday briefing of the White House COVID-19 Response Team. "Our biggest concern is we are going to continue to see preventable cases, hospitalizations and sadly deaths among the unvaccinated."
Ironically, just a few weeks after she made that statement, Ms. Walensky would go on CNN and concede the vaccines were ineffective at stopping community spread of COVID-19.
Fully vaccinated people who get a COVID-19 "breakthrough" infection can spread the virus to others even if they are not symptomatic, Centers for Disease Control Director Rochelle Walensky told CNN on Thursday.
She warned that an autumn/winter surge in the COVID "Delta" variant could again see hundreds of thousands of cases per day.
"Our vaccines are working exceptionally well," she said. "They continue to work well with 'Delta' with regard to severe illness and death, but what they can't do anymore is prevent transmission.”
Even as the narrative shift from the failed “vaccines will ‘crush' the virus” to “vaccines will keep you from getting very sick and going to the hospital” unfolded, the messaging remained unapologetically tilted in favor of the vaccines as the pathway back to “normal” society. Highly optimistic claims about the vaccines ability to protect against severe COVID-19 symptoms were made repeatedly (which makes the six months the Dror study languished in peer review limbo nothing if not suspicious, as it just happened to be the six months when the vaccines were being pushed the hardest).
In July of 2021, the Israeli Health Ministry claimed the Pfizer vaccine was highly effective at preventing hospitalization and severe COVID-19, even as it conceded the vaccine was only 39% effective against infection.
Pfizer and BioNTech’s Covid-19 vaccine is just 39% effective in Israel where the delta variant is the dominant strain, but still provides strong protection against severe illness and hospitalization, according to a new report from the country’s Health Ministry.
The efficacy figure, which is based on an unspecified number of people between June 20 and July 17, is down from an earlier estimate of 64% two weeks ago and conflicts with data out of the U.K. that found the shot was 88% effective against symptomatic disease caused by the variant.
However, the two-dose vaccine still works very well in preventing people from getting seriously sick, demonstrating 88% effectiveness against hospitalization and 91% effectiveness against severe illness, according to the Israeli data published Thursday.
In October of 2021, a study conducted by Pfizer and healthcare provider Kaiser Permanente claimed the Pfizer vaccine remained highly effective for up to six months against COVID-19.
Pfizer and healthcare provider Kaiser Permanente looked at records from 3.4 million residents of southern California, about a third of whom were fully vaccinated between December 2020 and August 2021.
After an average period of three to four months, fully vaccinated people were found to be 73% protected against infection and 90% protected against hospitalisation.
In December, 2021, right before the new year, doctors in South Africa published a letter to the editor of the New England Journal of Medicine stating the Pfizer vaccine remained “highly effective” even against the “Omicron” wave then sweeping the country.
During the proxy omicron period, we found a vaccine effectiveness of 70% (95% confidence interval [CI], 62 to 76), a finding that was supported by the results of all sensitivity tests. This measure of vaccine effectiveness was significantly different from that during the comparator period, when the rate was 93% (95% CI, 90 to 94) against hospitalization for Covid-19 (Table 2).
Nowhere among any of these claims was a role for vitamin D even mentioned.
These claims themselves are, of course, open to challenges of accuracy, but given that such challenges would only reduce the efficacy percentages, for the purpose of comparing these claims against the Dror study results, we can take them at face value. These efficacy percentages are the “best case" for the vaccines at preventing hospitalization and severe COVID-19 symptoms.
This “best case" for the vaccines is they were 88-93% effective against hospitalization for the Delta variant, falling to 70% effective against the Omicron variant.
By comparison, the Dror study indicates that vitamin D prophylaxis would be ~93% effective against hospitalization and ~94% effective against mortality. In other words, vitamin D is every bit as effective as the vaccines.
While the Dror study might be among the most optimistic, it is not the only study showing vitamin D's capacity to ward off COVID-19 hospitalizations.
The Demir study discussed above indicated vitamin D was 89.3% effective at preventing severe COVID-19,
The Jude study published in June of 2021 indicated that vitamin D was 71.6% effective against hospitalization.
The Karanova study published in January of this year after being submitted just in December showed vitamin D intake was 94.6% effective against hospitalization.
Thus, even taking the vaccine claims at face value, the best that can be said of the vaccines is they are just as good as vitamin D at warding off severe COVID-19 symptoms and hospitalizations. When one considers the short duration of the vaccines’ efficacy and the need for boosters, the vaccines quickly fall to second place compared to vitamin D.
Vitamin D, of course, invites none of the risk for myocarditis, pericarditis, or any of the other adverse events documented for the vaccines in VAERS. Quite the contrary, vitamin D is an essential nutrient apart from its utility in mitigating COVID-19. That fact alone makes vitamin D very attractive in dealing with COVID-19.
Neither Rochelle Walensky, Anthony Fauci, nor any of the countless “experts” appearing in the legacy media have discussed any of this. Their narrative has been exclusive advocacy in favor of vaccination.
Good Health Is Always The Best Defense
As seemingly impressive as some of the vitamin D statistics are, ultimately even they are merely a side note to a more important point: the best protection against severe COVID-19, or any severe infectious respiratory disease is always a healthy immune system. Even the vaccines operate by purportedly strengthening the immune system.
The difference is vitamin D unquestionably succeeds at accomplishing that.
It should be understood that even vitamin D supplementation will not stop COVID-19 in its tracks. Infection still happens. Still, a 14-fold reduction in hospitalizations and a 17-fold reduction in mortality would have greatly altered public perception of the pandemic. Even a 19% reduction in hospitalizations and the duration of hospital stays—the overall effectiveness of vitamin D shown in meta-analysis across a wide body of research—would have sufficed to significantly alleviate the burdens on hospitals.
Moreover, vitamin D is readily available in this country as an over the counter nutritional supplement. It is demonstrably cost effective—one shudders to think how many free vitamin D supplements could have been distributed for the billions that have been spent on the less effective and more dangerous vaccines.
If the goal is to stop COVID-19 in its tracks, then there are no “magic bullets”. Even the vaccines fail miserably in that regard.
But if the goal is the far more realistic effort to manage and mitigate an endemic respiratory pathogen, then good health is always going to be the best defense. Vitamin D plays a significant role in achieving that good health, particularly good immunological health, along with a healthy diet, exercise, and good restorative sleep—all the things we should already know are necessary to properly care for our bodies.
That is a message we have never heard from Anthony “the science” Fauci, Rochelle Walensky, or any of the media's self anointed “experts”—and likely never will, to their eternal shame and professional humiliation.
If vitamin D is fairly to be considered a “magic bullet” for making COVID-19 manageable, by ignoring it the “experts” have truly shot themselves in the foot with it.








Vitamin D is in the same league as any number of other, cheap, readily available things that could have made the "pandemic" more manageable. HCQ, IVM, Fluvoxamine, antihistamines, nigella sativa, all either ignored or actively disparaged as prophylaxis and early treatment.
"Manageable" is clearly not what The Powers That Be wanted.
When you look at the graph from Quraishi et al. 2014 (all refs at https://vitamindstopscovid.info/05-mds/) showing proper immune function only above 50 ng/mL 25-hydroxyvitamin D, and realise that most people (without proper supplements) have 1/2 to 1/10th this, then you can clearly see that vitamin D supplementation can bring about highly significant benefits to most people. No other nutrient is generally so deficient or easy, safe and inexpensive to replete.
Any doubts about the urgency of repleting people's 25-hydroxyvitamin D to at least this level evaporate when Chauss et al. 2021 is considered - Th1 regulatory lymphocytes from the lungs of severe COVID-19 patients drive constant inflammation (indiscriminate cell destruction) indefinitely. They fail to switch from their pro-inflammatory cytokine producing startup program to their anti-inflammatory shutdown program, even after each cell detects the conditions to do so. The primary or sole cause is that the cells lack sufficient
25-hydroxyvitamin D .
It is not good enough to take the lousy 800 to 2000 IU vitamin D3 cholecalciferol many doctors recommend (for 70 kg 154 lb bodyweight). This will never get most people's 25-hydroxyvitamin D levels to or over 50 ng/ml (125 nmol/L). For this average adult bodyweight, without obesity, 0.125 mg vitamin D3 a day is required. This is 5000 IU - an IU is 1/40,000,000th of a gram, the amount a baby mouse needs each day to avoid the bone weakening disease of rickets.
70 to 100 IU per kg bodyweight is ideal, so 5000 to 7000 IU a day. I am 69 kg and take 1.25 mg 50,000 IU a week. I guess my 25-hydroxyvitamin D level is between 50 and 100 ng/mL, which is fine.
Even with this proper daily supplementation (food and multivitamins have very little vitamin D - and UV-B skin exposure causes DNA damage and so raises the risk of skin cancer) it takes months to boost the long-lasting (1 or 2 month half-life) store of 25-hydroxyvitamin D in the the bloodstream, as measured in vitamin D blood tests.
Bolus vitamin D3 (such as 10 mg 400,000 IU as a single dose, again for 70 kg bodyweight) still takes 4 days or so to raise 25-hydroxyvitamin D levels from typical ~10 to ~20 ng/ml levels safely over 50 ng/mL. This is because the vitamin D3 needs to be hydroxylated in the liver.
By far the best form of early treatment - for anyone with COVID-19, sepsis, Kawasaki disease, MIS-C etc. and who has not been properly supplementing vitamin D3 for months - is a single oral dose of calcifediol, which is the pharma name for 25-hydroxyvitamin D. 0.014mg / kg bodyweight means ~1mg for 70 kg. This raises 25-hydroxyvitamin D levels over 50 ng/mL in 4 hours. This is the main reason for the success of the Castillo et al. RCT with hospitalised COVID-19 patients in Cordoba, Spain. 0.532 mg calcifediol, with half this on days 3, 7, 14 etc. (vitamin D3 would have worked just as well to maintain the boosted levels) reduced ICU admissions from 50% to 2% and deaths from 8% to zero. (The randomisation turned out to be unbalanced, so some of this extraordinary outcome is due to that, rather than the treatment.)
Most MDs have no idea about 25-hydroxyvitamin D being an essential requirement (at 50 ng/mL or more) for the autocrine (within each cell) and paracrine (to nearby cells) signaling systems by which each individual immune cell, of multiple types, responds to its changing circumstances.
Fortunately, calcifediol is now available without prescription - as small tablets of 0.01mg. 100 of these is 1mg and it is easy for most people to take these a few at a time. Alternatively they can be made into a drinkable slurry (best for children) with water and a little xanthan gum: https://nutritionmatters.substack.com/p/calcifediol-to-boost-25-hydroxyvitamin .
Doctors Paul Marik, Pierre Kory, Joseph Varon and colleagues at the Frontline COVID-19 Critical Care consortium now recommend bodyweight based long-term vitamin D3 supplementation in their I-MASK+ home treatment and I-RECOVER long COVID protocols: https://covid19criticalcare.com/covid-19-protocols/ .
Their hospital treatment MATH+ protocol recommends 0.014 mg / kg bodyweight single oral dose calcifediol as the best way of rapidly repleting 25-hydroxyvitamin D, with bolus vitamin D3 second. They should also mention the need for daily vitamin D3 to maintain the initially boosted levels from calcifediol. They recommend this for "COVID-19, sepsis, Kawasaki disease, Multisystem Inflammatory Syndrome, Acute Respiratory Distress Syndrome, burns, and vitamin D deficiency in early pregnancy or other clinical emergencies. This is so safe that there is no need to test 25-hydroxyvitamin D levels first. Toxicity cannot occur from this single dose, unless the person already has 150 ng/mL or more 25-hydroxyvitamin D levels - which can only be reached by weeks or months of highly excessive vitamin D3 supplementation.
Although Omicron typically causes less harm in low vitamin D people than Delta and previous variants, it is still a crap-shoot with a potentially destructive virus. While the FLCCC recommend calcifediol or bolus vitamin D3 for hospital treatment, it is the best possible early treatment for people who have not already been supplementing vitamin D3 properly for months - the earlier the better.