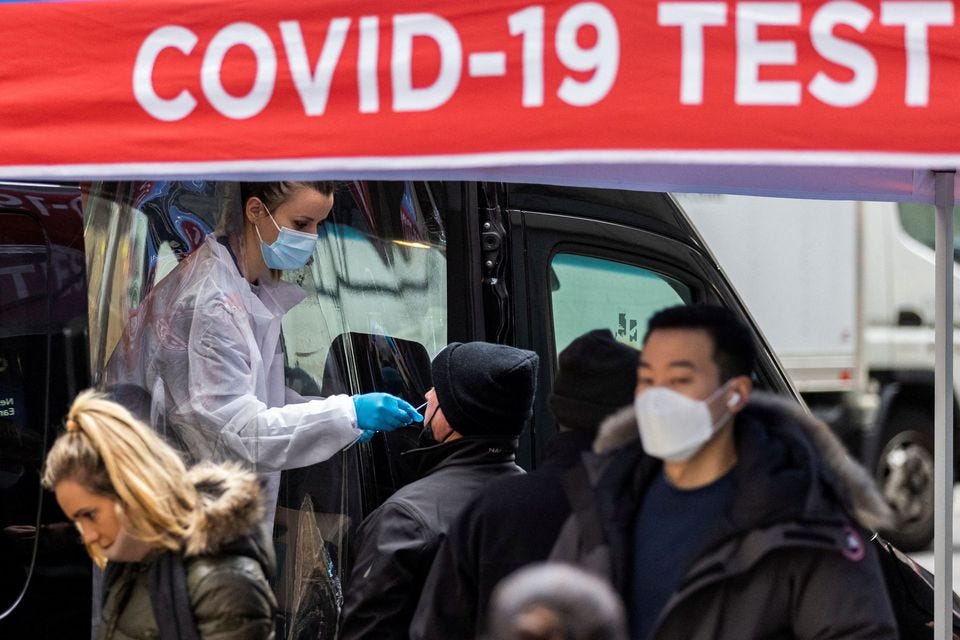
Followers of my Minds and Telegram channels have already seen my observations regarding claimed “surges” in COVID-19 hospitalizations, and the discrepancy between the claims reported by a feckless and supine media and what even the “official” data shows.
Yet time and again we are seeing reports in the media that are simply not borne out by even a cursory review of the actual data. Here are just a few of the dubious reports:
On December 9, New Hampshire was reported to be down to the last 3% of their ICU beds statewide—a claim not supported by the hospitalization data maintained by the Department of Health and Human Services.
On December 10, New York Governor Kathy Hochul instituted a new face mask mandate, citing a surge in hospitalizations that HHS data cannot confirm.
On December 8, Ohio news media reported the state was running out of hospital beds. The HHS data shows plenty of spare capacity statewide.
On December 13, we were treated to California Governor Gavin Newsom imposing a mask mandate due to a “surge” in cases—in a week when case numbers showed a noticeable decline.
At issue is not whether cases or hospitalizations are rising or falling, but whether the severity of the situation is being adequately presented. There is also a question of whether COVID-19 is in fact the driving dynamic; as I have discussed previously, hospitalizations for non-COVID causes are on the rise as well.
The failure of the media to contextualize their reporting with essential data leaves their pandemic panic narrative a study in unreality.
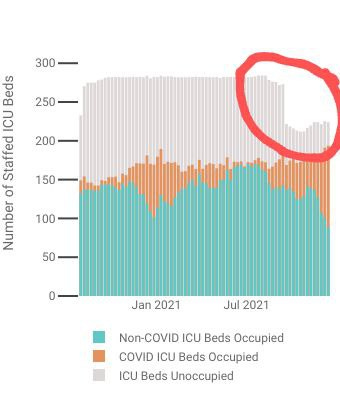
New Hampshire: The Missing Bed Mystery
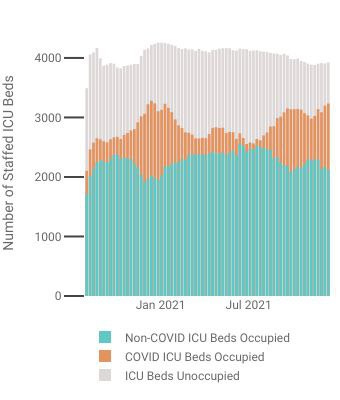
WMUR News painted an unquestionably dire picture of the state of New Hampshire hospitals: according to the state health department, as of December 9, the state was running out of staffed Ibeds because of rising COVID-19 hospitalizations.
As COVID-19 hospitalizations rise, the state is seeing intensive care unit beds fill. Several hospitals now say they no longer have any ICU beds available.
According to the New Hampshire Department of Health and Human Services, only 2.6% of staffed adult ICU beds are available statewide.
Left unmentioned, however, was a 51-bed drop in total staffed ICU beds in September—23% of total capacity.
It is intuitively obvious that a one-fourth reduction in capacity will result in an higher utilization percentage. Yet WMUR did not explore the reasons for the drop (and, lacking data as to the cause, I will not speculate on it here).
Even so, according to the Federal Department of Health and Human Services data, at the time of the WMUR report, New Hampshire ICU beds statewide were at 88% capacity, and as of the most recent reporting period, are at 89% capacity.
While COVID-19 hospitalizations are up significantly in the state, according to the data reported to and then by HHS, the rise is well within state capacity thus far. The crisis WMUR reported on December 9 did not exist, nor does it exist as of this writing, based on the HHS data.
Why did New Hampshire reduce its ICU beds capacity? Why has it not restored that capacity? These are important questions wholly ignored by the media. For now, those missing ICU beds remain a mystery.
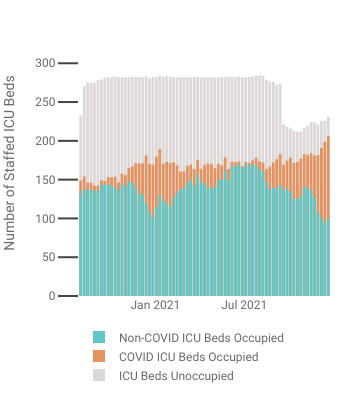
New York: The Phantom Surge
At almost the same time as New Hampshire's non-crisis, New York Governor Kathy Hochul instituted a new face mask mandate, complete with criminal sanctions. The reported rationale was concerning over rising COVID-19 cases and hospitalizations.
The statewide seven-day average case rate has increased by 43% since Thanksgiving and hospitalizations are up 29% in that timeframe, the governor said. Vaccinations have increased 2% in that window, not enough to outpace the spread.
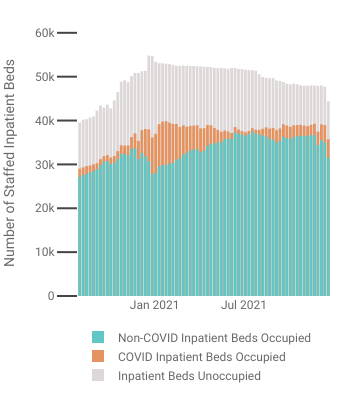
I shall concede an important detail up front: cases and hospitalizations for COVID-19 are up in New York. However, even with the rise, HHS data shows the state staffed inpatient bed capacity at 82% for the week covering the report of the mandate.
As of this writing, inpatient bed capacity is at 81%, with far more available beds than those occupied by COVID-19 patients.
Equally significant and equally ignored is the overwhelming majority of New York hospital beds occupied by non-COVID patients. Those other healthcare issues surely should be a factor in government policy regarding the public health, yet there is no acknowledgement by the media these issues even exist.
Yet they do exist, and because they exist, and because of New York's overall inpatient capacity, Governor Hochul's “surge” in COVID-19 hospitalizations truly does not exist within the HHS data. Her mask mandate is defending against a phantom surge, not addressing the maintenance of New York's public health.
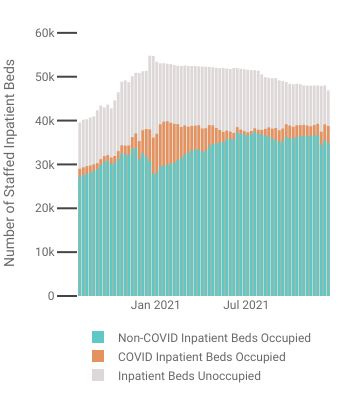
Ohio Can't Find Any Hospital Beds. Perhaps They Should Look In The Hospitals
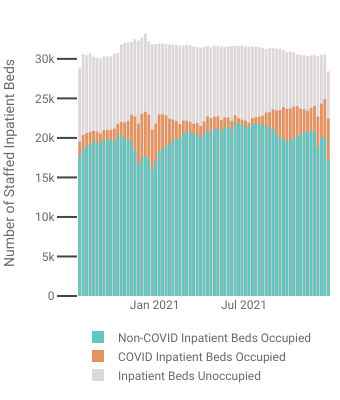
Meanwhile, the Buckeye State has been reporting difficulty finding hospital beds their COVID-19 patients.
The COVID-19 pandemic has turned into a desperate search for hospital beds across Ohio, as well as efforts to avoid hospitals being overwhelmed with patients.
Medical centers are returning to their 2020 pandemic playbooks, and turning to strategies such as postponing elective surgery, transferring patients to other hospitals, and refusing new emergency department patients.
Looking at the HHS data, however, perhaps they should look in their hospitals, which reported ample staffed bed capacity to HHS.
At the time of the media reporting, Ohio ICUs were at 82% capacity, with 1,117 COVID patients and 688 spare ICU beds. Overall, Ohio hospitals were reporting at 81% capacity, with 4,680 COVID patients and 5,732 spare hospital beds.
As of this writing, Ohio ICUs are still at 82% capacity, with 1,224 COVID-19 patients and 696 spare ICU beds. Overall, Ohio is reporting hospital beds at 79% capacity, with 5,161 COVID-19 patients and 5,966 spare beds.
If Ohio cannot find hospital beds for its patients, perhaps they just aren't looking in the right hospitals. Statewide they have plenty of beds, according to the HHS data.
California: What Goes Up Also Comes Down
When Gavin Newsom imposed a new mask mandate on California, the stated rationale was (of course) rising COVID-19 cases.
Gov. Gavin Newsom’s administration announced the new mandate will start Wednesday and last until Jan. 15. The order comes as the per capita rate of new coronavirus cases in California has jumped 47% in the past two weeks.
However, cases in California began trending sharply down after December 9 and had been trending down generally for about a week prior.
Even looking at the latest revisions to the case numbers, it is clear that the rise in cases had ended by the time Governor Newsom acted on them.
The case numbers in California highlight an inevitable limitation of mandates in responding to a public health issue: disease does not wait on bureaucracy, leaving government invariably two steps behind any disease, including COVID-19. This bit of context has never appeared in the media reporting on the pandemic.
Cases Are Rising. That Does Not A Crisis Make.
As even alt-media sources have noted, COVID-19 cases are rising in the US, particularly in the northeast, which, ironically, is one of the country's more heavily inoculated regions.
Admissions involving patients with COVID climbed 14.4% across the US in the week ended Dec. 9, according to the US Department of Health and Human Services. In New England, the rate was more than double - 33.5%.
This latest surge is happening in what is perhaps the most vaccinated area of the US. In Massachusetts, where 88% of the population has had at least one dose of the vaccine, the state is planning to send out more than 2MM rapid antigen tests to the poorest communities, according to Gov. Charlie Munger.
Yet rising case numbers and hospitalizations are only part of the pandemic picture.
A proper appreciation for the burden these rises place on the healthcare infrastructure necessarily includes an understanding of the capacity of that infrastructure. When a state has one in five ICU or inpatient beds available, a rise in hospitalizations is not public health crisis.
Similarly, rising cases are a concern, but falling cases are a relief. Effective policy needs to address both trends, or risk becoming non-responsive to a constantly changing situation.
Follow The Data
The only way to rationally assess any situation is to look at the data, and comprehend how that data ebbs and flows during any crisis. What the data shows today is not for certain what the data will show tomorrow. As any situation unfolds, the data surrounding that situation will change, and plans and strategies must adapt accordingly.
For its part, the media has a professional and ethical obligation to reflect the changing data. The media needs to follow the data, for when they become wedded to a narrative, the result is propaganda, which serves no one.
Those wishing to take prudent steps with regards to the pandemic should follow the data as well, with or without the media narrative. As these “phantom surges” demonstrate, the narrative is never the reality. Only the data can be that.