Remember: It's All "Just The Flu"
The Term "Influenza Like Illness" Exists For A Reason
As summer moves into fall, we once again move into that time of year historically described as “cold and flu season”. Perhaps we might update that to “cold, flu, and COVID season”, given the high attention now being paid to the coronvirus SARS-CoV-2 and its attendant infections.
Regardless of how we approach the labeling, this much will never change: Colds, influenza, RSV (respiratory syncytial virus), as well as COVID are all diseases caused by infectious respiratory pathogens, and all fall under the CDC rubric of “Influenza Like Illness”.
Bear that in mind when reading the corporate media regurgitation of its Pandemic Panic Narrative, which would have you believe that COVID is still a major public health crisis.
The COVID-19 pandemic feels like a thing of the past, but recent spikes in cases and the appearance of a brand new variant across four continents are reminders that the pandemic is far from over.
Do not be seduced by their intimations of grave public health threat from COVID.
It may feel like pandemic déjà vu: New Covid-19 variants are afoot, and hospitalizations are again on the rise. One called Eris became the most prevalent in July, followed by another dubbed Pirola, which has been detected in 10 countries including the US and UK as of Aug. 30. The US Centers for Disease Control and Prevention and the World Health Organization are closely monitoring the situation. For now, experts aren’t too concerned, though the UK is starting its fall Covid vaccination 2023 booster a month early due to the increased risk.
While individuals will always need to take precautions appropriate for their overall level of health and well-being, the data is quite clear: for the past year at the very least the impact of COVID on public health infrastructures has been minimal.
Like colds, flu, and RSV, COVID is, ultimately still “just the flu”. It’s still one type of Influenza Like Illness.
First, let us be clear what we mean when we say “Influenza Like Illness”.
The CDC defines “Influenza Like Illness” as any illness which presents with a fever, cough, and/or sore throat.
ILI is defined as fever (temperature of 100 °F or greater) and cough and/or sore throat. It is used for flu surveillance worldwide.
If we look at the CDC’s list of symptoms for COVID, we see that COVID unequivocally fits that definition.
Influenza (Flu) itself of course fits this definition, based on the symptoms:
Flu Symptoms
Influenza (flu) can cause mild to severe illness, and at times can lead to death. Flu symptoms usually come on suddenly. People who have flu often feel some or all of these symptoms:
fever* or feeling feverish/chills
cough
sore throat
runny or stuffy nose
muscle or body aches
headaches
fatigue (tiredness)
some people may have vomiting and diarrhea, though this is more common in children than adults.
Even Respiratory Syncytial Virus (RSV) fits this definition, based on the symptoms.
Symptoms
People infected with RSV usually show symptoms within 4 to 6 days after getting infected. Symptoms of RSV infection usually include
Runny nose
Decrease in appetite
Coughing
Sneezing
Fever
Wheezing
In a very real sense, they are all “just the flu”. This does not mean they are mild or that they are incapable of posing a serious threat to an individual’s health and well-being. All infectious respiratory pathogens have the potential to produce severe symptoms and severe illness. A case of “the flu” may be mild or severe, regardless of whether the underlying pathogen is SARS-COV-2, Influenza, RSV, or some other virus producing these symptoms.
Yet while an individual case of “the flu” may be mild or severe, the public health impact of cases of “the flu” are typically minimal. The CDC data sets demonstrate this in abundance.
On a nationwide basis, combined Emergency Department visits for COVID, Flu (Influenza) and RSV never exceeded 10% of all ED visits.
Even if we break it down by state, such as in California, we still do not see all respiratory virus activity accounting for more than 10% of ED visits.
Illinois saw a higher combined percentage at 14% of all ED visits, but COVID visits did not exceed the national average of 4%. Flu visits were by far the major source of ED visits.
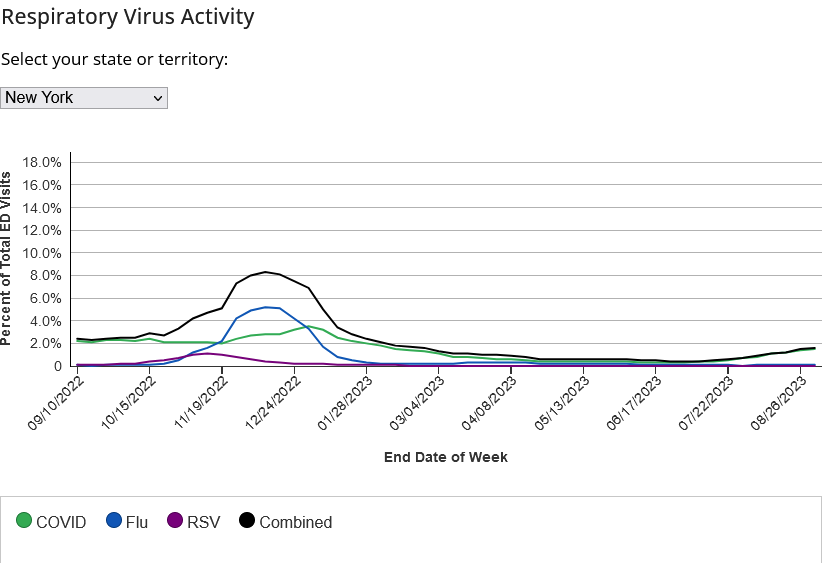
Pick any state, such as New York, and the trend holds: Flu accounts for more ED visits than COVID at their respective peaks.
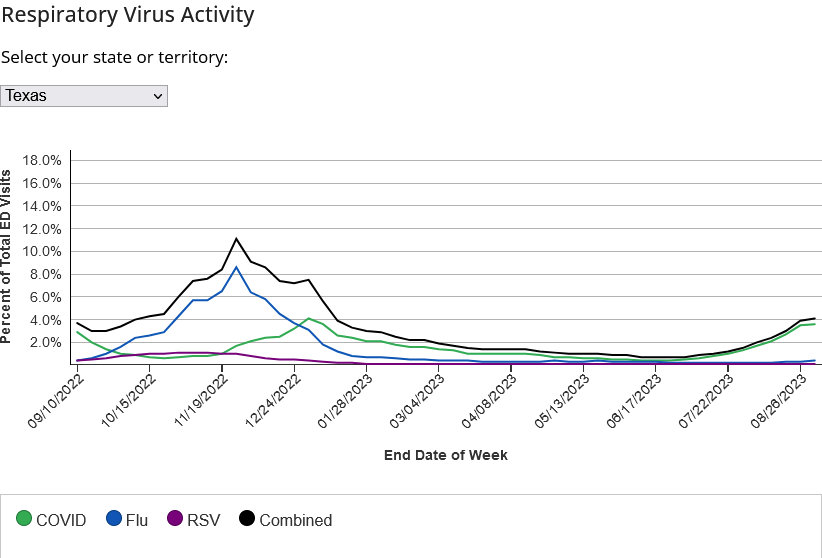
This is true even in notionally politically conservative states such as Texas.
Respiratory viruses are completely apolitical. They don’t care about the host’s politics, only his or her vulnerability to infection.
No matter how one views the data, the end result is the same—COVID and “the flu” present in largely the same way, and at approximately the same time.
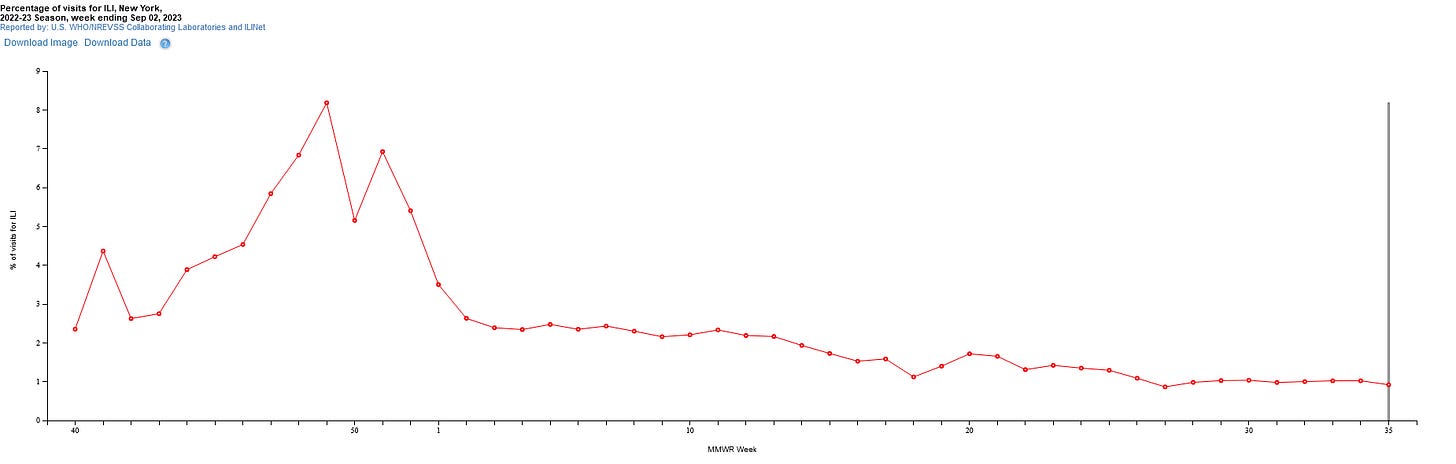
When we view the CDC’s “FluView” chart on flu cases in California, we see a mid-November 2022 peak.
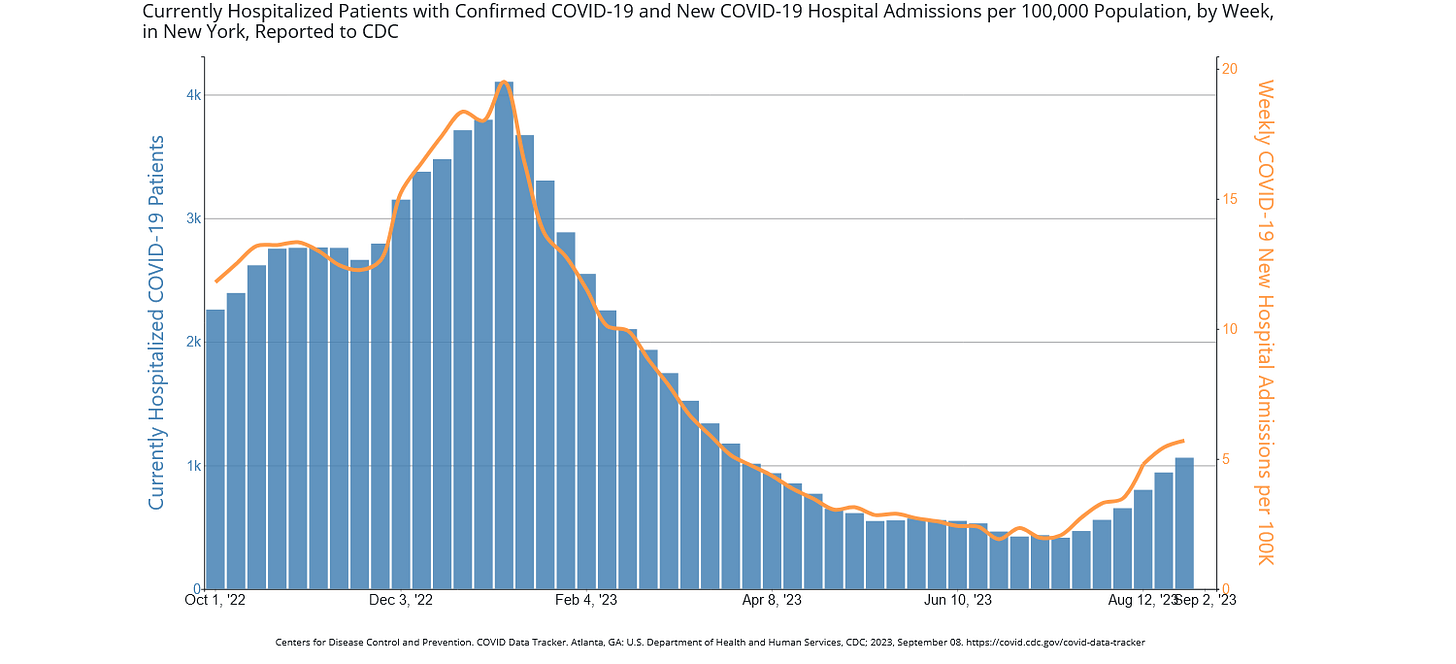
If we look at the CDC’s COVID data, we see that COVID hospitalizations peaked just a little bit later, in December, but that the cases for both COVID and the flu follow broadly similar trajectories.
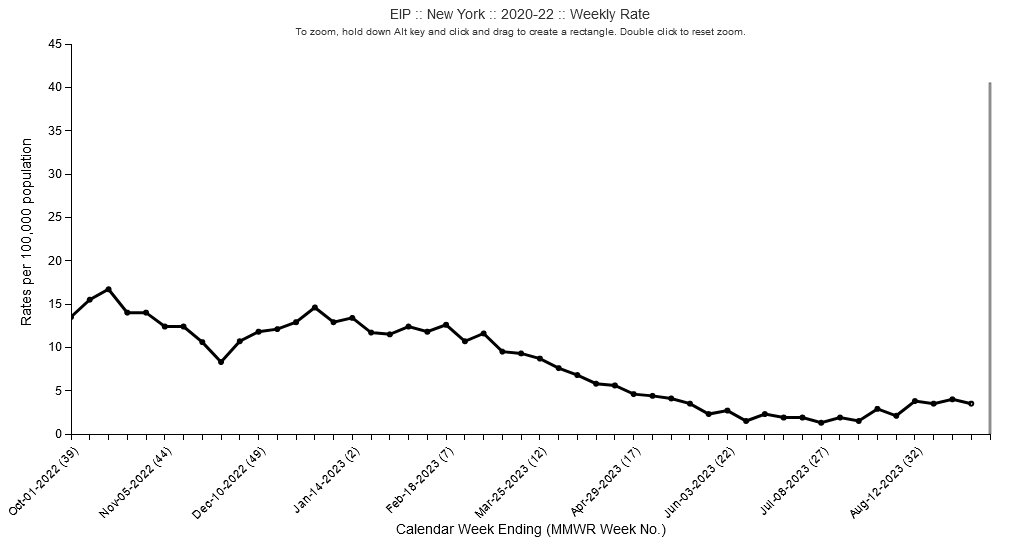
If we look at New York, we again see the same broad patterns and trends.
COVID hospitalizations on a nationwide basis have been, for the past year, fairly low.
Even in New York, the hospitalizations per 100,000 people have not exceeded 17 in the past year.
As has been documented by the CDC throughout the “pandemic” and ever since, by far the major determinant of whether or not a case of COVID (or, for that matter, a case of influenza or RSV) is likely to become severe and result in hospitalization and/or death is the presence of comorbid conditions.
As of August 20, 2023, only 5% of COVID deaths presented with no comorbidities recorded.
Table 3 shows the types of health conditions and contributing causes mentioned in conjunction with deaths involving COVID-19. The number of deaths that mention one or more of the conditions indicated is shown for all deaths involving COVID-19 and by age groups. For over 5% of these deaths, COVID-19 was the only cause mentioned on the death certificate. For deaths with conditions or causes in addition to COVID-19, on average, there were 4.0 additional conditions or causes per death. For data on deaths involving COVID-19 by time-period, jurisdiction, and other health conditions
With an average of 4 comorbid conditions involved in COVID deaths, it is no exaggeration to say that the sicker one is at the time of infection, the more likely it is COVID will become a serious illness. Age also plays a role, as elderly patients are far more vulnerable that young adults.
The same is broadly true of all respiratory illnesses.
The SARS-CoV-2 virus is here to stay. Regardless of where it originated, the virus is now endemic worldwide. There will be seasonal outbreaks of COVID cases just as there are seasonal outbreaks of influenza and RSV. The data makes that abundantly clear as well.
Yet this also means that SARS-CoV-2 is not any great cause for alarm in and of itself. Certainly those who are immunocompromised or immunodeficient will need to take special care to avoid infection—but this is true for all infectious respiratory pathogens. Nor should anyone be blithe and careless about getting sick—even for a healthy person getting “the flu” has a fairly high suckage factor attached.
What SARS-CoV-2 is not is a reason to upend one’s life. What SARS-CoV-2 is not is the second coming of the Black Plague, or even the Spanish Influenza of 1918-1919, certainly not at the present time. The data does not lend itself to even a passing comparison between current iterations of SARS-CoV-2 and those prior true pandemic diseases.
Summer is slipping into fall. That means we are slipping into cold season. We are slipping into flu season. We are slipping into RSV season. We are slipping into COVID season. This we do every year right about this time.
Be smart about your health. Be protective of your health. Take reasonable and prudent precautions to avoid getting sick, not just from COVID, but from any disease.
But be realistic about such diseases. The CDC terms these illnesses “Influenza Like Illness” for a reason—they are largely indistinguishable from one another going by symptoms alone.
In a very real and substantive way, COVID is still, just as it has always been, “just the flu.”











"even for a healthy person getting “the flu” has a fairly high suckage factor attached."
But it is still better than the shot, any shot, especially the mRNA shot. As a former Heath Professional, retired now, I only received a single flu shot back in 1981, (the boss, a PharmD talked me into it), I felt so bad from that single injection that I laid on the porch in the hopes that one of my buddies would stop by and put me out of my misery. Alas, no one did, and then, about 6-7 hours later, I made a remarkable recovery.
Now, we can speculate what the flu shot did, or didn't do, but I have not taken another since.
Excellent article, should be required reading for anyone contemplating a flu shot, unless it is some version of the mRNA, then pictures of it's carnage should be included.
Excellent piece!
I've always believed that Covid was simply the flu "rebranded".
Unvaxxed, and not gonna get a flu shot.
I simply take care of my immune system...