Monkeypox has clearly been selected to be the next official virus of the Pandemic Panic Narrative.
Emergencies Emerge
After the WHO's Director General unilaterally decided that monkeypox spreading across Europe and North America without (at the time) causing any deaths was a Public Health Emergency of International Concern (but 75 suspected deaths from monkeypox in Africa was not an emergency of any kind), now three states have joined the WHO in viral lunacy.
On Friday, Governor Kathy Hochul declared a state of emergency over the spread of monkeypox within the state, announcing her decision via Twitter.
Earlier that same day, Brazil and Spain announced the first deaths outside of Africa from the virus. Brazil’s death was a 41-year old patient also suffering from cancer.
On Monday, Illinois and then California declared states of emergency over the disease. New York City Mayor Eric Adams also declared a state of emergency within the city. The statements and the rationale behind each declaration more or less mirrored Governor J B Pritzker’s Tweet announcing the declaration:
The narrative for monkeypox has thus been set: it’s real bad, real scary, real dangerous, so everyone must be vaccinated at once against it.
That’s the narrative. What does the data say about the disease?
Monkeypox By The Numbers
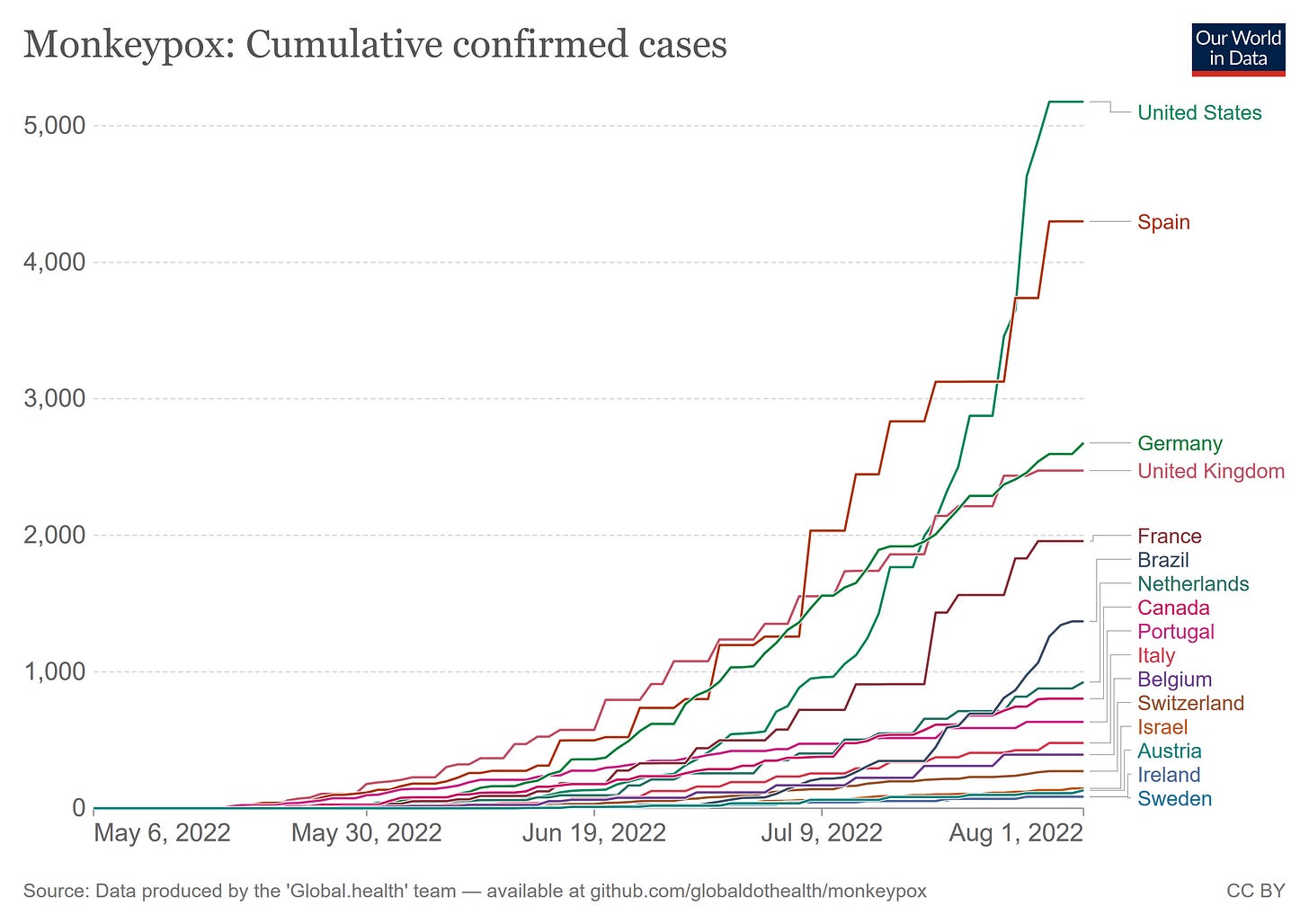
As of August 2nd, the CDC reported 25,391 cases of monkeypox worldwide.
6,326 of those cases are in the United States. 99% of US cases are among gay and bisexual men, many of whom had recently traveled abroad. Intimate and sexual contact is the primary vector by which the virus appears to be transmitted outside of Africa1.
Many of the initial patients reported international travel in the 21 days prior to symptom onset, visiting countries not known to experience endemic monkeypox and participating in large festivals and other activities where close, personal, skin-to-skin contact likely occurred. Recent travel history does not confirm the person acquired their infection while traveling. Since late June, an increasing number of reported cases have been linked to local community transmission.
After approximately July 27, the United States has had the majority of monkeypox cases recorded.
With the WHO recording a total of 7 deaths2 from Monkeypox, it is not a disease to simply be ignored, particularly in the United States, but outside of Africa, monkeypox is presenting as a sexually transmitted disease that is impacting almost exclusively gay and bisexual men—not quite the broad basis one might think necessary for a disease to become a Public Health Emergency of International Concern.
Don’t Say Gay: Public Health Officials Most Concerned About “Stigma”
As the emergency declarations in New York, Illinois, and California make clear, public health officials and the corporate media are most concerned with avoiding any semblance of “stigma” regarding the virus’ apparent preference for gay and bisexual men.
Although anyone can get infected, the outbreak appears to have largely affected men who have sex with other men. That's led some public health officials to question how to raise awareness about the spread without making the early public health mistakes of the HIV/AIDS crisis when gay and bisexual men were stigmatized and discriminated against.
As part of this effort to avoid “stigma”, public health “experts” are advocating minimizing the reality that 99% of cases are among gay and bisexual men.
It's a tricky conversation but it matters, said Dr. Joseph Lee, a professor of health education and promotion at East Carolina University who has studied public health messaging.
"We need to make sure we're getting the right people involved in reaching the right communities and saying things in a way that resonates," Lee told NPR. "Because the harm of getting it wrong is real and hard to repair.
In particular, pointing out that intimate sexual contact appears to be the driving force spreading the virus has been deemed unhelpful, and suggesting that refraining from sexual activity until the outbreak has subsided is inappropriate patient teaching.
Joaquín Carcaño, the director of community organizing at the Latino Commission on AIDS, said that guidance is not only ineffective but can pose more risk.
"We know abstinence-only education doesn't work for pregnancy, so why would we use it for this?" he told NPR. "When you say no sex, you're mischaracterizing that MPV, also known as monkeypox, is a sex-associated transmission, which it can be, but it's not the end all be all."
However, this stance, as I have noted previously, flies in the face of the clinical research into the outbreak which has established unambiguous associations between sexual activity—and in particular promiscuous sexual is activity—and spread of the virus.
The suspected means of monkeypox virus transmission as reported by the clinician was sexual close contact in 95% of the persons. It was not possible to confirm sexual transmission. A sexual history was recorded in 406 of 528 persons; among these 406 persons, the median number of sex partners in the previous 3 months was 5 partners, 147 (28%) reported travel abroad in the month before diagnosis, and 103 (20%) had attended large gatherings (>30 persons), such as Pride events. Overall, 169 (32%) were known to have visited sex-on-site venues within the previous month, and 106 (20%) reported engaging in “chemsex” (i.e., sex associated with drugs such as mephedrone and crystal methamphetamine) in the same period.
With a median number of 5 sexual partners in a 3 month period, and frequent instances of “chemsex” among individuals infected with monkeypox outside of Africa, sexual promiscuity is absolutely established as part of the transmission vector. Just don’t say that out loud, especially if you are an healthcare professional.
Monkeypox Vaccines Do Not Exist
While public health “experts” from the WHO to state and local public health officials are advocating monkeypox vaccination as the best means of curtailing monkeypox spread, one key fact is glaringly absent from that part of the narrative: there is no monkeypox vaccine.
The vaccine that is being urged on people, JYNNEOS™ is a live, non-replicating, vaccinia virus vaccine originally designed as a smallpox vaccine. While it is approved for vaccination against monkeypox, its efficacy as a monkeypox vaccine has never been rigorously tested or studied.
From the CDC Monkeypox vaccination web page (emphasis mine):
Because Monkeypox virus is closely related to the virus that causes smallpox, the smallpox vaccine can protect people from getting monkeypox. Past data from Africa suggests that the smallpox vaccine is at least 85% effective in preventing monkeypox. The effectiveness of JYNNEOS™ against monkeypox was concluded from a clinical study on the immunogenicity of JYNNEOS and efficacy data from animal studies.
“Immunogenicity” means the vaccine was tested by measuring antibody production—and that testing was done with a view towards its use as a smallpox vaccine.
Serum antibody titers were measured with the use of a plaque-reduction neutralization test (PRNT) and an enzyme-linked immunosorbent assay (ELISA). The vaccinia-specific PRNT and ELISA used the vaccinia virus Western Reserve strain and MVA, respectively, as antigens; the detection limits were titers of 2 and 50, respectively.
Given the rarity of monkeypox exposure prior to 2022, direct testing of Jynneos against actual monkeypox exposure has not been possible3. This makes everyone receiving the Jynneos vaccine in the US part of a large, albeit uncontrolled, experiment into its actual efficacy against monkeypox—one in which the participants have no opportunity for informed consent.
This fact is not one you will find in the corporate media reporting on monkeypox, where the narrative is “vaccines work against monkeypox”. That assertion has to be considered essentially false at this point, for the simple reason that, without direct testing of Jynneos against actual monkeypox exposure, its actual efficacy as a monkeypox vaccine is, ultimately, unknowable. It produces antibodies shown to neutralize smallpox, which is a close cousin of monkeypox, and the use of a prior smallpox vaccine (ACAM2000) in Africa to protect against monkeypox was found to be 85% effective while generating similar antibody titers, but how well Jynneos works against monkeypox can only be inferred at this point.
Does this mean Jynneos won’t work against monkeypox? No, it does not. It does mean that there is a large degree of uncertainty about how well it will work. ACAM2000’s observed 85% effectiveness alone makes the use of a smallpox vaccine as prophylaxis against monkeypox somewhat problematic, and the reliance on Jynneos having similar immunogenicity to ACAM2000 makes its use even more problematic. While it is unlikely to be wholly ineffective, whether it will even be 85% effective against monkeypox is still largely a matter of educated guesswork at this point.
Monkeypox Is Similar To Herpes
Let us say the quiet part out loud: monkeypox is a sexually transmitted disease just as herpes is.
The herpes simplex virus is considered a sexually transmitted disease by the CDC, and spreads via contact with active sores and lesions—the exact same transmission modality ascribed to monkeypox. If herpes qualifies as an STD, then so too must monkeypox, even though transmission via semen or vaginal secretions has not been conclusively established.
While the sexual act itself is not necessary to transmit the virus, the close, skin-on-skin contact that is necessary is of an intimate and sexual nature.
What makes this understanding relevant is the reality that, just as promiscuous sex increases the spread of STDs, sexual restraint (and abstinence) decreases its spread. Avoiding close, intimate, sexual contact with infected individuals is by far the best means available to avoiding a case of monkeypox. Where there is no exposure there can be no transmission.
This cannot be said in the corporate media openly because to do so would be to “stigmatize” gay and bisexual men—or so the narrative would have us believe. This is, of course, total malarkey. Sexual promiscuity is the behavioral concern, not homosexuality vs heterosexuality.
Monkeypox Is A Concern. It Is Not An Emergency
The declarations of monkeypox as a public health emergency are, in every instance, simply asinine. Even with the known fatalities in Brazil and Spain (and, soon enough, elsewhere), it is still not an emergency. It does not have the mortality of HIV, nor does it appear to result in recurring infection vis-a-vis herpes.
The facts show monkeypox is best apprehended as a serious sexually transmitted disease, and the mitigation for STDs remains sexual restraint. Sexual promiscuity of any kind is simply not healthy. It has never been healthy.
Monkeypox does not present a case for mass vaccination, especially with a vaccine that is essentially untested. While monkeypox may be related to smallpox, it is not smallpox. It does not present the mortality risk associated with smallpox. It does not warrant using anyone as glorified guinea pigs for vaccine testing without their explicit consent.
Perhaps the argument would be different if the basis for the global outbreak was the Central African clade of the virus as opposed to the far less dangerous West African clade. Perhaps then the virus would present a better case for mass vaccination.
Perhaps.
Yet the global outbreak is derived from the West African clade, the less dangerous strain of the virus. That is the epidemiological reality before us.
Monkeypox is a legitimate public health concern. It is not a public health emergency, nor is it likely to become one.
From the WHO Situational Report of 25 July 2022:
“In the African region, the latest data on monkeypox shows an increase in cases since April 2022, compared to the same period in 2021. From 1 January to 8 July 2022, there have been 2087 cumulative monkeypox cases, of which only 203 were confirmed. The overall case fatality ratio for the 203 confirmed cases is 2%. Of the 175 confirmed cases for which there are case-specific data, 53% were male and the median age was 17 years, making the demographics of cases in Africa similar to recent previous outbreaks but significantly different from other Regions.”
The WHO breakdown of monkeypox deaths has not yet incorporated the reported death in Brazil.
Given the potential even for the West African clade of monkeypox to be lethal, a clinical trial for Jynneos involving deliberate infection with the virus would be unethical in the extreme. However, papering over that lack of direct testing against actual monkeypox exposure and simply presenting the inferred efficacy as established fact is itself an unethical act, as it denies vaccine recipients the opportunity for truly informed consent.