Monkeypox: The Non-Emergency Public Health Emergency
The 2022 Global Outbreak Is Already Fading
The virtue signalers are not going to be happy about this, but monkeypox, which was never a true public health emergency, is already fading away.
The WHO, the CDC, and the European Centers for Disease Control (ECDC) are all reporting the same thing: fewer monkeypox cases—a lot fewer.
The Global Outbreak Is Receding
In their most recent Situation Report dated 24 August, the WHO reports that monkeypox cases are down 21% worldwide.
During the week of 15 to 21 August, the number of cases reported in the Region of the Americas shows a continuing steep rise, confirming trends seen over the last several weeks. Globally, after four consecutive weeks of increase, the number of monkeypox cases reported declined by 21% overall during the same week (n=5907 cases) as compared to the previous week (n=7477 cases). This decrease may reflect early signs of a declining case count in the European region, which would need to be subsequently confirmed.
While the WHO does claim a “steep rise” in cases in the Region of the Americas, their own graphic suggests otherwise, with cases actually moving onto a plateau in that region.
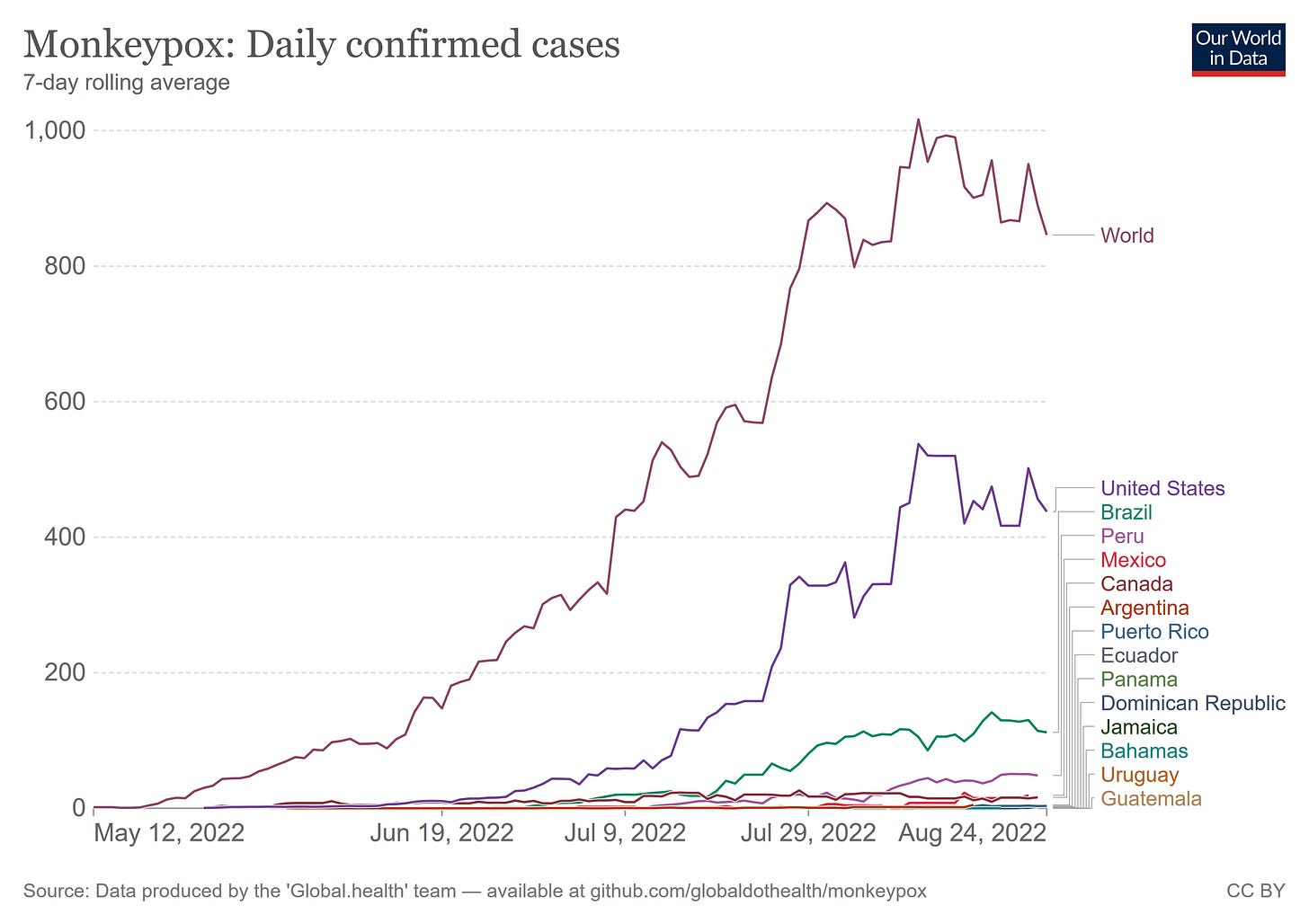
Moreover, independent epidemiological data from Our World In Data shows a decline in cases within the Western Hemisphere:
This decline in cases is mirrored by the data gathered by the CDC, as both the 7-day and 14-day moving averages for newly reported cases in the US are on the decline.
Meanwhile, the ECDC data shows the monkeypox outbreak there crested in mid-July and has declined dramatically since.
Viewed globally, monkeypox is fading away.
Even the African outbreak, which presents far differently both in terms of transmission and overall mortality, appears to be on the wane, with few new cases reported in the most recent Outbreaks And Emergencies Bulletin.
Virtue Signalers Gonna Virtue Signal
The decline in cases has not stopped the virtue signalers from continuing their shrill “monkeypox is scary!” narrative, however, with absurd and utterly unrealistic comparisons to COVID-19 and HIV the prevailing norm.
But as the alarm and case counts grow, it is increasingly clear that the U.S. and the global communities are repeating some of the hallmark failures of other global health crises, such as the COVID-19 pandemic and the HIV/AIDS epidemic. From mounting stigma and misinformation, to botched testing and vaccine rollouts, to the widening inequities in care, the parallels between Monkeypox, COVID-19 and HIV/AIDS should cause officials to reevaluate and redirect their approach to this latest public health emergency.
What are the parallels between monkeypox, COVID-19, and HIV/AIDS? There are none, propaganda efforts to the contrary notwithstanding.
The propaganda, for example, denies that the global outbreak of monkeypox is a sexually transmitted disease.
For example, many news reports refer to monkeypox as a sexually transmitted disease that only impacts the gay community. Both parts of this statement are false, yet the misinformation continues to reverberate in a disturbing echo of the discrimination against LGBTQ+ communities during the HIV/AIDS epidemic.
When you look at the data, however, both parts of that statement are unquestionably true. From the WHO’s own Situation Report:
The outbreak continues to affect young people of male gender, with 98.2% (20 138/20 500) of cases with available data on the gender being males with a median age of 36 years (Interquartile range: 30-43 years). Fewer than 1% (140/23 626) of cases with age data available are aged 0-17 years. This proportion differs between countries, with those in West and Central Africa reporting a greater proportion of cases among young age groups: 38.7% (65/168) of cases for whom age was available were among the age group 0-17, out of which 12.5% (21/168) were aged 0-4.
Among cases with sexual orientation reported, 95.8% (9484/9899) identified as men who have sex with men. Of all reported types of transmission, a sexual encounter was reported most commonly, with 5954 of 7250 (82.1%) of all reported transmission events.
The majority of cases were likely exposed in a party setting with sexual contacts, with 2204 of 3639 (60.6%) of all likely exposure categories.
Among cases with known HIV status, 45% (4501/10 036) are HIV positive.
Moreover, observational data throughout the outbreak has consistently supported sexual activity among gay and bisexual men as the primary transmission vector for the global outbreak1.
Vaccines Have Not Been Relevant
Of course, no edition of the Pandemic Panic Narrative would be complete without the obligatory call for “vaccination, vaccination, and more vaccination”.
The larger issue is still the paucity of the JYNNEOS vaccine for monkeypox, but the Administration for Strategic Preparedness and Response (ASPR) is in charge of the national stockpile.
The agency's decision last week to use one vial of JYNNEOS to protect five people is a step in the right direction, but what we really need is millions more vaccines. The Department of Health and Human Services has ordered 5.5 million more doses from Bavarian Nordic with 2.5 million of these to be filled and finished by a U.S. manufacturer, but the delay will still be months.
However, the much-bemoaned shortage of the JYNNEOS vaccine serves only to underscore what is almost certainly the primary contributor to the decline in cases in the US: non-pharmaceutical behaviorial alterations by the most at-risk population of gay and bisexual men.
As is generally the case with sexually transmitted diseases, alterations in sexual behavior away from promiscuity and towards discretion are the most effective means for slowing and even stopping the spread of monkeypox.
This reality is reflected in the preparations being made for increased wastewater surveillance for monkeypox in New Orleans, which is gearing up for the “Southern Decadence” LGBTQ festival held each year in the French Quarter:
There have been 151 reported monkeypox cases in Louisiana so far, with the majority of those – 111 – in the New Orleans area. Experts expect to see a spike in levels from wastewater collected during Southern Decadence, with presumably a slump after.
“The whole thing with Southern Decadence will be very interesting,” said Dr. Julio Figueroa, professor and chief of infectious diseases at LSU Health New Orleans. “It will be interesting to see how much of that spike goes away after Decadence.”
The expectation that increased sexual activity will result in increased monkeypox spread reflects the assessment of New Orleans’ public health experts that shifts in behavior patterns impact monkeypox spread. What shifts in one direction can be shifted in another direction as well.
Every Virus Is Going To Virus, And Then Fade Away
That monkeypox is receding even without a massive public health effort is unsurprising. Outbreaks are so-called because pathogens come and then they go. They rarely disappear completely, but they do recede into the background for a time.
Viruses infect, they virus, they spread, they run out of vulnerable hosts, and then they subside again.
This is a recurring theme among viruses. Just as the SARS-CoV-2 virus spreads and then fades, so, too, is monkeypox.
As Brian Mowrey noted in his “Unglossed” Substack the other day, even the dreaded 1918 Spanish Influenza virus has never actually left us.
Monkeypox was never going to do anything but what it is doing now—fade away as it runs out of vulnerable hosts, which is happening because people are choosing to make themselves less vulnerable. Vaccines are not the reason for this ebb and flow, but simple and fairly basic self-care.
The lesson to be learned from monkeypox is the same as the lesson we should have learned from COVID-19: we are our own best defense against infectious disease.
As I have discussed previously, the African outbreak should be viewed and considered separately from the global outbreak, as the modes of transmission and mortality risk are vastly different. Thus I refer to the spread of monkeypox outside of Africa as the “global outbreak”.












Good points, but I think they aren't done with monkeypox yet...I just read today about kids getting it in Atlanta - https://www.wsbradio.com/news/local/new-case-numbers-show-least-3-kids-under-age-17-georgia-have-contracted-monkeypox/DU3QYSBUHJGYRK6TSWEJTDB2C4/